sponsored content
November 15, 2023
By Nicholas Gidosh, OD
AccuLens’ NewVision corneo-scleral orthokeratology lens has received FDA clearance for daily wear. The large diameter design provides comfort to the patient, with four distinct zones: base curve/optic zone, reverse curve zone, corneal alignment curves, and corneal-scleral curves. All parameters of the lens can be adjusted independently of each other to ensure clear vision, comfortable wear, and a custom fit for each patient.
Benefits of a Larger Lens
As a practitioner, what I find to be great about the NewVision lens design is that it’s based on data. The design is based on elevation points we’re measuring with our topography or profilometry, making it analogous to what people are already used to for fitting scleral lenses. With scleral lenses, we care about the sagittal depth of the eye to land on the sclera, but with OrthoK, we’re landing typically inside the cornea.
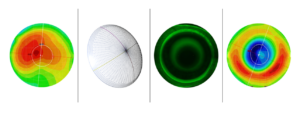
What we’re doing with NewVision is measuring points of elevation across the corneal surface, and by having a larger design, we’re going to land in the peripheral cornea — like a traditional OrthoK lens. Because it’s larger, the edges will extend beyond the limbus. We don’t want to have the lens bearing on the limbus — it will have a landing point inside the cornea. If you’re looking at a fluorescein pattern, you’re going to expect to see a fluorescein flush or glow beyond the limbal points over to the sclera. So, the NewVision lens is bigger than what people are used to in terms of an OrthoK lens, but it’s still very similar.
The Acculens New Vision uses a scleral design for both fit and comfort. There are two main benefits of the lens being larger. With a larger design, the lens is going to give better centration. It will be more tucked under the upper and lower lids. Part of what makes a GP lens uncomfortable is that as the patient blinks, their lid margin is going back and forth over the edges of the lens, and that’s what they feel. When dealing with an OrthoK lens 10.5-11 mm in diameter, that’s not the entire aperture. When you compare that to a larger trans-limbal kind of design, it will be tucked under that upper and lower lid. After the patient blinks, they’re not going to have that margin of their eyelid going back and forth over the edge of the lens.
Another benefit of having a larger diameter is that it’s going to help center the lens on the eye. It’s a very common change in OrthoK, especially in the case of a lens decentering laterally. If it decenters towards the nasal or temporal sides, usually one of the first things we do is go larger. However, if we start with a larger design already, it should give us better centration and more first lens success when fitting.
Customizing the Lens for Each Patient
The diameter of the lens is customized for each patient based on the diameter of their eye. If a patient has a larger corneal diameter, they will end up with a larger lens. As a result, if they have a smaller corneal diameter, they will end up with a smaller lens, so that customization matches the size of the cornea. The different zones will reflect that as well. That’s another bonus about going with a larger lens — if a patient has a large pupil, one of the issues we run into is that the patient can sometimes end up with aberrations or glare and have real difficulty with that at nighttime. Having a larger design that we can customize to be larger to match the size of the pupil is a benefit — especially for older patients who are interested in OrthoK.
Data is Key
The old saying, “garbage in, garbage out,” really comes into play when practitioners consider fitting this lens. We need good data to work from. If you’re using profilometry or topography, you want to get good scans of the cornea, make sure the surface isn’t dry, and make sure that you get as much data as you can. Be sure to capture the peripheral data as well. It’s important that we have a good scan in the beginning to work from.
In terms of the fitting process, the fluorescein that you’re looking for looks just like a regular OrthoK pattern. It’s just going to be a larger lens. You’re looking for that glow over the lens edge over your limbus to make sure that you have good tear exchange and you’re not sealed off or crushing down on the limbus.
More Research is Underway
The NewVision lens has received clearance from the FDA for daytime wear, which is unique for an OrthoK lens. However, as practitioners who prescribe OrthoK as a means of controlling myopia progression, that is also an off-label use. With the NewVision lens, we’re still using it off-label, just in a different way.
Currently, Acculens is working on a study aimed at assessing the efficacy of wearing the lenses overnight, and that is awaiting approval from the Internal Review Board (IRB). Once we get that approval, we’ll start recruiting patients into the trial to ensure that there are no issues with wearing a large design in an overnight modality. The ultimate goal is to gain full and total FDA approval for the NewVision lens.
 |
Nicholas Gidosh, OD, is an Assistant Professor at the Pennsylvania College of Optometry (PCO). Dr. Gidosh graduated from PCO with Honors and went on to complete a Cornea and Contact Lens residency at the Michigan College of Optometry at Ferris State. After three years in private practice, he returned to serve as Chief of the Cornea and Contact Lens Service (CCLS) at The Eye Institute (TEI). Since then, he has presented lectures and workshops in PCO’s Advanced Studies Program and International Program, with topics including scleral and hybrid lenses, irregular cornea, and contact lens fitting. Dr. Gidosh is a Fellow of the American Academy of Optometry and has served as a clinical investigator for studies involving hybrid, scleral, multifocal, and OrthoK lenses, presenting lectures and posters at national and international conferences on these topics. Dr. Gidosh’s current areas of research are in optimizing scleral lens optical and fitting designs for patients with irregular corneas. He also researches and lectures on myopia control strategies, particularly Orthok as it pertains to patients with astigmatism. |