August 2, 2021
By Sally Dillehay, OD, EdD, FAAO, Expert Content Contributor for the Brien Holden Vision Institute Global Myopia Center
Deciding when to start treatment for myopia is clinically a matter of assessing the risks for each child with the treatment goals of keeping the refractive error as low as possible and the axial length below 26 mm.

A recent analysis of data from almost 6,900 children in the U.S. demonstrated that age and female sex were the most significant factors related to whether or not a child develops myopia and the amount of myopia that occurs.1 These findings are consistent with published data demonstrating that the progression of myopia is faster at younger ages2 and that an earlier onset of myopia leads to a higher amount of myopia due to a greater number of years of active progression of myopia.3
Given the substantial amount of evidence that continues to build that it is important to prevent or delay the onset of myopia as long as possible, a simple answer to the question of when to start myopia treatment is as early as possible, perhaps even while the child is still considered a “pre-myope,” a term defined by the International Myopia Institute as:4
“A refractive state of an eye of ≤ 0.75 D and > 0.50 D in children where a combination of baseline refraction, age, and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions.”
While treatments for pre-myopes currently would most likely consist of recommending increased outdoor time due to limited published evidence in this group and the fact that visual correction is not yet likely to be required,4 when should you start considering an optical or pharmaceutical treatment strategy for those children who have already developed myopia?
Understanding What Factors Impact Myopia Progression
The Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error study, which followed almost 5,000 children ages 6 to 14 for more than 10 years, demonstrated if a child’s refractive error at age 6 years old is < +0.75D, age 7-8 < +0.50D, age 9-10 < +0.25D, and age 11 < 0.00D,5 that child should be closely monitored for the development of myopia. Additionally, the fastest rate of refractive error change in myopic children will occur in the year just before the onset of myopia.6
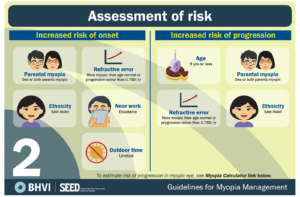
A child who has a less plus/more minus refractive error than those listed for his/her age has an 80% likelihood of developing myopia by the age of 13.7 As part of a decision to begin treatment based on a child’s age, and refractive error status, eye care professionals must also consider the presence of other risk factors such as family history of myopia,8 the amount of time spent outdoors,9 the child’s visual environment,9 and the child’s binocular vision status.10
Download this chart here.
Additionally, a child who is progressing in myopia at a faster rate should also be considered at higher risk for developing a higher level of myopia. In these children, earlier treatment is warranted to attempt to keep the final level of myopia under approximately -5.00D, in which the risk for sight-threatening visual complications later in life increases.11 The average amount of annual myopic progression varies by age and ethnicity.12 Clinically, a child progressing -0.50D to -0.75D per year or more would be more likely to be considered a faster progressor. More frequent examination intervals with earlier commencement of treatment would be warranted.
How does the measurement of axial length fit into the decision to begin treatment for myopia? Although some average growth charts have been published for both Asian and European Caucasian children,13 the use of these charts and axial length measurements is not straightforward. Age, ethnicity, and refractive status can all impact the axial length and its elongation over time.13 One can use the published growth charts by age to see if a child’s axial elongation is in a higher percentile than predicted for his/her age. Emmetropic children demonstrate approximately 0.10 mm of axial length increase per year.14 Therefore, one possible use of axial length measurements in the determination to begin treatment may be if the observed axial elongation is greater than that amount. While the use of axial length measurements may be confounded by age, ethnicity, and refractive status, including corneal curvature, generally, a desirable treatment goal is to maintain an axial length of less than 26 mm, in order to avoid risks of potential vision loss later in life.15
The Importance of Eye Exams
All children, regardless of their refractive error status, should be examined at least once between the ages of 3-5 to establish baseline measurements and the presence of risk factors for the development of myopia.16 Additionally, all children should be examined at least annually until they are age 18,16 as myopia does continue to progress for a large percentage of children even after age 15.17 Current clinical recommendations are that all myopic children age 12 or less should be treated for myopia, and pre-myopic children should at a minimum be provided with information regarding risks for the development of myopia and the need to spend sufficient time outdoors.16
Deciding when to start treatment for myopia is clinically a matter of assessing the risks for each child with the treatment goals of keeping the refractive error as low as possible and the axial length below 26 mm.16 Age, parental myopia, ethnicity, the amount of near work, and the amount of time spent outdoors are additional risk factors that should be taken into consideration when developing your treatment strategy and goals.

Dr. Dillehay is the President of ClinTrialSolutions, LLC, a medical research organization helping to bring innovative medical devices to market through research and clinical trials, including several in the area of slowing the progression of myopia. She serves as an Expert Content Contributor for the Brien Holden Vision Institute Global Myopia Center.
References
1 Harb, EN, Wildsoet, CF. Nutritional Factors and Myopia, Optom Vis Sci May 7, 2021 – Volume Pre-Publication. DOI: 10.1097/OPX.0000000000001694.
2 Chua SY et al. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Opthal Physiol Opt 2016;36:388-94.
3 Sankaridurg, P.R. and B.A. Holden, Practical applications to modify and control the development of ametropia. Eye (Lond), 2014. 28(2): p. 134-141.
4 Flitcroft DI, He M, Jonas JB et al. IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Invest Ophthalmol Vis Sci 2019; 60, M20-M30.
5 Zadnik K et al. Prediction of Juvenile Onset Myopia. JAMA Opthalmol 2015;133:683-899.
6 Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci2007;48:2510-2519.
7 World Health Organization – Brien Holden Vision Institute. The impact of myopia. In: The Impact of Myopia and High Myopia. Report of the Joint World Health Organization–Brien Holden Vision Institute Global Scientific Meeting on Myopia.
8 Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P.Outdoor Activity Reduces the Prevalence of Myopia in Children. Ophthalmol 2008;115:1279-1285.
9 Mutti, D.O., et al., Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci 2002. 43(12): p. 3633-3640.
10 Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A Ratio, Age, and Refractive Error in Children. Invest Ophthalmol Vis Sci 2000;41:2469-2478.
11 Haarman AE et al. The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthalmol Vis Sci 2020; 9;61:49
12 Brennan NA et al. Influence of Age and Race on Axial Elongation in Myopic Children. Optom Vis Sci 2018; 95: eAbstract 180072.
13 Wolffsohn JS, Kollbaum PS, Berntsen DA, et al. IMI – Clinical Myopia Control Trials and Instrumentation Report. Invest Ophthalmol Vis. Sci2019;60(3): M132-M160.
14 Chamberlain, P, Lazon de la Jara, P, Arumugam, B, Bullimore, MA. Axial length targets for myopia control. Ophthalmic Physiol Opt 2021; 41: 523– 531.
15 Tideman JW, Snabel MC, Tedja MS et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol 2016; 134:1355-63.
16 Mastering Myopia Clinical Guide (Dec 2020). Accessed July 10, 2021 at https://covalentcreative.s3.amazonaws.com/jjv/media/documents/Managing_Myopia_Clinical_Guide_Dec_2020.pdf.
17 Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-465.













