May 14, 2019
By Kevin Chan, OD, MS, FAAO
Treehouse Eyes
The prevalence of myopia and high myopia are increasing in the U.S. and globally at an alarming rate, with significant increases in the risks for vision impairment from pathologic conditions associated with high myopia, including retinal detachment, myopic macular degeneration, cataract, and glaucoma. Over 30 percent of the world is currently myopic, and by 2050, almost 50 percent will be myopic … a staggering 5 billion people. The US has an estimated overall prevalence of 42 percent in the 12 – 54-year-old age group, almost doubling in three decades. In children and teenagers ages 12-17, the total U.S. prevalence of myopia is estimated to be a shocking 34 percent1,2.
The alarming progression of myopia in East Asia has resulted in more than 20% of the population to develop pathologic myopia 6,7. The public health consequences of myopia have become far too serious to be neglected, considering the increasing risks of vision-threatening complications and global economic burden associated with myopia. Notably, myopic macular degeneration has shown to severely impact visual impairment and functioning 3,4,5, which indirectly resulted in a massive loss of productivity worldwide 8.
Managing low myopia in young adults who continue to progress more than 0.50D per year past age 18
The onset age of myopia among children and adolescents is directly linked to its rate of progression 9,10, which can potentially be predictive of further myopia development in adulthood. While it has been commonly perceived that myopia stabilizes upon cessation of growth spurts as early as age 15 12, interestingly, recent research has found that age at axial length (AL) stabilization lacks association with gender, ethnicity, or number of myopic parents 11. In other words, AL may increase past puberty and continue elongation during adulthood, resulting recurrence of myopia progression.
While young children with predisposing risk factors of myopia, such as two myopic parents, Asian descent, are more likely to develop higher myopia in adulthood 13,14, it is not uncommon to notice young adults with low myopia continue to experience a gradual relapse of myopia progression, yet generally at a relatively slower pace. This growing trend was found to more likely to develop signs of posterior degeneration of the retina 4,6,15.
Undoubtedly, gene-environmental interactions play a vital and definite role in myopia development 16-19. In particular, the study by Tideman et al. found that genetic loci relating to myopia likely exert its effect as a function of age among children, adolescents, and adults 15. Among these three age categories, the adult group aged 25 or above have shown to have the highest number of loci associated with AL and corneal radius (CR). This suggests that myopia development and progression in adults likely occur more commonly than previously expected.
I am often asked about whether young adults showing progressive myopia can be treated with overnight orthokeratology lenses. While young adults are generally more inclined to excel better with orthokeratology lenses because of greater dexterity and tolerance, they also have higher expectations for the quality of vision compared to children. The overall treatment outcomes associated with orthokeratology lenses are primarily influenced by patients’ motivation, compliance, and wear time. Be mindful when selecting young adult patients with type-A personality and fluctuating sleep schedule. Extensive education and discussion with adult progressive myopes before initiating treatment is crucial in developing an understanding of their preferences and expectations. Orthokeratology treatment for adult progressive myopes has shown to successfully reduce, or in some cases halt, refractive error and axial elongation progression, even upon discontinuation of treatment 23.
Managing myopia in a 22-year-old professional student with adult-onset myopia
In comparison to early onset of myopia in children and adolescents, emmetropic adults who suddenly experience myopic spike, especially when they are in graduate or professional studies, are particularly intriguing. Studies have shown that ocular biometric factors, such as diurnal choroidal and quadrant-specific macular thickness, are significantly varied in young adult myopes compared to emmetropes 21,22,33,33. For young professionals who were formerly emmetropic, increased number of years of education has shown cumulative effects in the higher incidence of myopia development in adults, but not in opposite manner 20. It is essential to evaluate these patients with a comprehensive cycloplegic examination and rule out the likelihood of pseudomyopia. Given the extensive demand of near work activities, young adults are likely to be susceptible to the aftereffects of nearwork, which can be a precursor to adult-onset myopia progression 24.
For cases like this, I typically prescribe soft contact lenses with a center-distance multifocal (MF SCL) design for new adult myopes since they are generally better accepted due to its convenience and excellent comfort. Nevertheless, MF SCL for myopia management is not without drawbacks. In the presence of peripheral plus power, the quality of vision may temporarily be affected with glare and low contrast sensitivity during initial adaptation 27,28. While these transient symptoms are generally well tolerated in the pediatric population, young adult myopes may view them as nuisances for which likely affect the overall adaptation and compliance. Typically, these symptoms subside in 1-2 weeks. Therefore, it is advisable to educate young adult patients about potential vision and glare adaptation with MF SCL and establish a realistic expectation for them.
In addition, the binocular vision function in young adults plays a crucial role in determining patient candidacy for myopia control treatments. Studies by Gifford et al. have shown that young adult myopes wearing orthokeratology lenses tend to display greater exophoria and lower accommodative lags compared to single-vision contact lens wearers 25,26. This explains why orthokeratology treatment may benefit young adult myopes with binocular vision dysfunction.
In the event of myopia progression that does not respond well to monotherapy treatment with an optical approach, low-dose atropine in combination with contact lens modality may be warranted. Despite a concentration-dependent response in slowing myopia progression and axial elongation in children 31, clinical efficacy of atropine in adult myopes is yet to be fully tested. In my experience, low-dose atropine, as little as 0.01%, is generally not considered as the first-line monotherapy treatment for young adults since they tend to be more noticeably impacted by the potential unwanted side effects of pupillary dilation and glare 29,30, as compared to children.
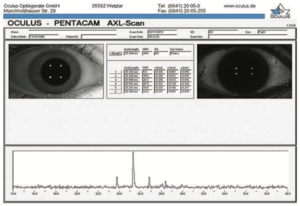
Pentacam Scheimpflug imaging system shown above. It is an important tool used for imaging and analysis of anterior segment and axial length (AL) measurement to help guide myopia management.
Managing expectations
When considering treatments for myopia management for young adults, it is essential to understand that this demographic generally represents young millennials with high education level and increased demand for the quality of vision. Optical approaches, such as orthokeratology and soft MF contact lenses, provide convenience and independence from glasses. Nevertheless, clinicians should also be mindful when setting realistic goals and expectations for each treatment. Given the long waking hours for school and work activities, visual clarity and stability are vital components in determining treatment success for young adults. Patients with variable sleep schedule or atypical work schedule (e.g., night-shift workers) may not be good candidates for orthokeratology. Meanwhile, we should also inform and educate patients who are sensitive to glare or halo about the potential adaptation with soft MF contact lenses and atropine. Otherwise, possible symptoms may outweigh clinical benefits.
Special considerations
Contrary to rapid progression in children and adolescents, the progression of adult-onset myopia in diopters generally acts less aggressively. However, due to a sustained period of axial elongation prior to adulthood, posterior choroid, sclera, and retina continuously experience physical stretching and insult, which may lead to more severe risks of myopic degeneration in young adults. Collectively, optical and pharmacologic approaches have shown to manage adult myopia effectively. Nevertheless, the absence of myopic degeneration does not necessarily indicate healthy, or ‘risk-free,’ retina. Practitioners should be prepared to step out of the ‘phoropter zone’ and familiarize with other clinical tools for myopia management. Axial length assessment at baseline and periodical intervals is highly recommended for determining prognosis and guiding treatment protocols. Furthermore, knowledge of macular and choroidal integrity found in OCT has shown promising application as potential biomarkers for myopia progression or development of myopia-related complications.
Bibliography
- Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016; 123:1036–1042.
- Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, Cook DG, Owen CG. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016 Jul;100(7):882-890
- Fricke TR1, Jong M, Naidoo KS, Sankaridurg P, Naduvilath TJ, Ho SM, Wong TY, Resnikoff S. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018 Jul;102(7):855-862.
- Wong YL, Sabanayagam C, Ding Y, Wong CW, Yeo AC, Cheung YB, Cheung G, Chia A, Ohno-Matsui K, Wong TY, Wang JJ, Cheng CY, Hoang QV, Lamoureux E, Saw SM. Prevalence, Risk Factors, and Impact of Myopic Macular Degeneration on Visual Impairment and Functioning Among Adults in Singapore. Invest Ophthalmol Vis Sci. 2018 Sep 4;59(11):4603-4613.
- Li Z, Liu R, Xiao O, Guo X, Wang D, Zhang J, Ha JJ, Lee JTL, Lee P, Jong M, Sankaridurg P, Ohno-Matsui K, He M. Progression of Myopic Maculopathy in Highly Myopic Chinese Eyes. Invest Ophthalmol Vis Sci. 2019 Mar 1;60(4):1096-1104.
- Wong YL, Saw SM. Epidemiology of Pathologic Myopia in Asia and Worldwide. Asia Pac J Ophthalmol (Phila). 2016 Nov/Dec;5(6):394-402.
- Pan CW, Dirani M, Cheng CY, Wong TY & Saw SM. The age‐specific prevalence of myopia in Asia: a meta‐ Optom Vis Sci 2015; 92: 258–266.
- Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, Sankaridurg P, Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis and modelling, Ophthalmology (2018).
- Greene PR1, Medina A Juvenile Myopia. Predicting the Progression Rate. Mathews J Ophthalmol. 2017;2(1).
- Zadnik K, Sinnott LT, Cotter SA, Jones-Jordan LA, Kleinstein RN, Manny RE, Twelker JD, Mutti DO; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol. 2015 Jun;133(6): 683-9.
- Hou W, Norton TT, Hyman L, Gwiazda J; COMET Group. Axial Elongation in Myopic Children and its Association with Myopia Progression in the Correction of Myopia Evaluation Trial. Eye Contact Lens. 2018 Jul;44(4):248-259.
- COMET Group Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013 Dec 3;54(13):7871-84.
- Chua SY, Ikram MK, Tan CS, Lee YS, Ni Y, Shirong C, Gluckman PD, Chong YS, Yap F, Wong TY, Ngo CS, Saw SM; Growing Up in Singapore Towards Healthy Outcomes Study Group. Relative Contribution of Risk Factors for Early-Onset Myopia in Young Asian Children. Invest Ophthalmol Vis Sci. 2015 Dec;56(13):8101-7
- Theophanous C, Modjtahedi BS, Batech M, Marlin DS, Luong TQ, Fong DS. Myopia prevalence and risk factors in children. Clin Ophthalmol. 2018 Aug 29;12:1581-1587.
- Tideman JW, Fan Q, Polling JR, Guo X, Yazar S, Khawaja A, Höhn R, Lu Y, Jaddoe VW, Yamashiro K, Yoshikawa M, Gerhold-Ay A, Nickels S, Zeller T, He M, Boutin T, Bencic G, Vitart V, Mackey DA, Foster PJ, MacGregor S, Williams C, Saw SM, Guggenheim JA, Klaver CC; CREAM Consortium When do myopia genes have their effect? Comparison of genetic risks between children and adults. Genet Epidemiol. 2016 Dec;40(8):756-766.
- Miraldi Utz V. Nature versus nurture: A systematic approach to elucidate gene-environment interactions in the development of myopic refractive errors. Ophthalmic Genet. 2017 Mar-Apr;38(2):117-121.
- Morgan IG, Rose KA. Myopia: is the nature-nurture debate finally over? Clin Exp Optom. 2019 Jan;102(1):3-17.
- Pozarickij A, Williams C, Hysi PG, Guggenheim JA1; UK Biobank Eye and Vision Consortium. Quantile regression analysis reveals widespread evidence for gene-environment or gene-gene interactions in myopia development. Commun Biol. 2019 May 6; 2:167.
- Ghorbani Mojarrad N, Williams C, Guggenheim JA. A genetic risk score and number of myopic parents independently predict myopia. Ophthalmic Physiol Opt. 2018 Sep;38(5):492-502.
- Mountjoy E, Davies NM, Plotnikov D, Smith GD, Rodriguez S, Williams CE, Guggenheim JA, Atan D. Education and myopia: assessing the direction of causality by mendelian randomisation. 2018 Jun 6;361: k2022.
- Xiao O, Guo X, Wang D, Jong M, Lee PY, Chen L, Morgan IG, Sankaridurg P, He M. Distribution and Severity of Myopic Maculopathy Among Highly Myopic Eyes. Invest Ophthalmol Vis Sci. 2018 Oct 1;59(12):4880-4885.
- Burfield HJ, Patel NB, Ostrin LA. Ocular Biometric Diurnal Rhythms in Emmetropic and Myopic Adults. Invest Ophthalmol Vis Sci. 2018 Oct 1;59(12):5176-5187.
- González-Méijome JM, Carracedo G, Lopes-Ferreira D, Faria-Ribeiro MA, Peixoto-de-Matos SC, Queirós A. Stabilization in early adult-onset myopia with corneal refractive therapy. Cont Lens Anterior Eye. 2016 Feb;39(1):72-7.
- Ciuffreda KJ, Wallis DM. Myopes show increased susceptibility to nearwork aftereffects. Invest Ophthalmol Vis Sci. 1998 Sep;39(10):1797-803.
- Gifford K, Gifford P, Hendicott PL, Schmid KL. Near binocular visual function in young adult orthokeratology versus soft contact lens wearers. Cont Lens Anterior Eye. 2017 Jun;40(3):184-189.
- Gifford KL, Gifford P, Hendicott PL, Schmid KL. Zone of Clear Single Binocular Vision in Myopic Orthokeratology. Eye Contact Lens. 2019 Apr 15.
- Kang P, McAlinden C, Wildsoet CF. Effects of multifocal soft contact lenses used to slow myopia progression on quality of vision in young adults. Acta Ophthalmol. 2017 Feb;95(1): e43-e53.
- Wahl S, Fornoff L, Ochakovski GA, Ohlendorf A. Disability glare in soft multifocal contact lenses. Cont Lens Anterior Eye. 2018 Apr;41(2):175-179
- Kaymak H, Fricke A, Mauritz Y, et al. Short-term effects of low-concentration atropine eye drops on pupil size and accommodation in young adult subjects. Albrecht von Graefe’s Archiv für Ophthalmologie. 2018;256(12):1-7
- Grzybowski A, Armesto A, Szwajkowska M, Iribarren G, Iribarren R. The Role of Atropine Eye Drops in Myopia Control. Curr Pharm Des. 2015;21(32):4718-30.
- Yam JC, Jiang Y, Tang SM, Law AKP, Chan JJ, Wong E, Ko ST, Young AL, Tham CC, Chen LJ, Pang CP. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. 2019 Jan;126(1):113-124.
- Duan F, Yuan Z, Deng J, Wong YL, Yeo AC, Chen X. Choroidal Thickness and Associated Factors among Adult Myopia: A Baseline Report from a Medical University Student Cohort. Ophthalmic Epidemiol. 2019 Apr 8:1-7.
- El-Shazly AA, Farweez YA, ElSebaay ME, El-Zawahry WMA. Correlation between choroidal thickness and degree of myopia assessed with enhanced depth imaging optical coherence tomography. Eur J Ophthalmol. 2017 Aug 30;27(5):577-584.











