May 3, 2021
By Katherine Schuetz, OD
The world is becoming more myopic, and we have a duty to reduce the complications that will follow those increasing numbers of longer eyes.

It’s a typical day at the office. You take a quick glance at the next chart before entering the room to meet the patient, a first grader who just failed his school screening with visual acuity of 20/50 OD, OS. It could be one of the many false positives we see from school screenings, particularly this year when ODs haven’t been able to access schools to volunteer due to the pandemic, or you could be about to give this child a first diagnosis of myopia. Defining this as life changing may sound extreme since we’re just talking nearsightedness of about -1.25D, but think about the lifelong implications in terms of quality of life, cost, and ocular health risk. Myopia is quite a big deal. How can you make this patient’s parents understand the implications?
My approach to explaining myopia is not exactly straightforward. Yes, I tell parents that their child needs vision correction to see clearly. I often demonstrate with trial lenses of +3.00D so parents can see what their -3.00D child sees uncorrected, but blurry vision is the easy explanation. Parents get that concept initially. Then parents inwardly groan as the realization sets in of the never-ending cost of new glasses and/or contact lenses every year for this child. Finally, the parent realizes their child will look “different” with glasses, and they’ve fallen into nostalgia and perhaps a little grief. You’ve completely lost any further opportunity to educate this family! This is why with myopic and “pre-myopic” children, we take axial length measurements at the time of the exam, and then we have them return approximately one month later after glasses are dispensed. That second follow-up is when I actually have the time to do more critical education, which is getting parents to understand that myopia is not a good thing from a health perspective.
The Importance of the Second Visit
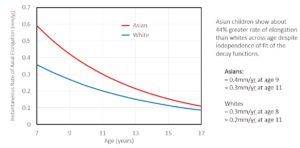
The second time I see a myopic child is when I can explain why parents’ genetics, child’s average outdoor time, refractive power, and the baseline axial length all matter in quite different ways than just needing glasses. Because we’ve already covered the glasses conversation and they’ve had time to process, now we can discuss that a myopic eye is longer than a typical healthy eye. Unfortunately, longer eyes have a significantly higher risk for retinal detachment, myopic maculopathy, cataracts, and glaucoma.1 I tell the parents that there is a virtual certainty that their child’s prescription will increase as they continue to grow. Still, the extraordinarily great news is that now we have options to slow myopia and eye elongation progression. We discuss that growing is essential, and all eyes grow during childhood, including eyes that don’t need glasses,2 but myopic eyes tend to grow faster, which we’d like to change.
 This second visit is when I will recommend a specific treatment option, which varies significantly depending on the child’s age, maturity, axial length, and refractive power. Again, the majority of parents will need time to process this information. Many parents are myopic themselves, which doesn’t necessarily make the conversation easier. Some will see their child’s myopia as a straightforward hassle that they can easily address via single vision glasses. Some will be terrified that their child’s vision will be “as bad as they are,” which will affect how quickly they will be ready to start their child with myopia management. Your job as the doctor is to show them the data regarding ocular health risks linked to myopia so that together you can get their child to a lower risk for complications in the future and be a better candidate for vision correction surgeries in adulthood if desired and appropriate.3
This second visit is when I will recommend a specific treatment option, which varies significantly depending on the child’s age, maturity, axial length, and refractive power. Again, the majority of parents will need time to process this information. Many parents are myopic themselves, which doesn’t necessarily make the conversation easier. Some will see their child’s myopia as a straightforward hassle that they can easily address via single vision glasses. Some will be terrified that their child’s vision will be “as bad as they are,” which will affect how quickly they will be ready to start their child with myopia management. Your job as the doctor is to show them the data regarding ocular health risks linked to myopia so that together you can get their child to a lower risk for complications in the future and be a better candidate for vision correction surgeries in adulthood if desired and appropriate.3
Presenting New Information
“Why have I never heard of this before?” is a valid parent question. The best answer is humbly explaining that we did not have a wealth of data and knowledge on myopia management until recently. For the past 100 years, eye doctors have steadily watched their patients become more nearsighted because we had no effective, consistent treatment beyond single vision spectacles and contact lenses. Why scare parents with morbid statistics about the risk of high myopia when we had no alternative to offer? Now we have the opportunity to keep this next generation of myopes at potentially shorter axial lengths and lower risk of vision-threatening eye disease.4
The key to myopia management for young myopes is in the doctor’s ability to convey the importance to the parents. If you are the only designated “myopia management” practitioner in your practice, make sure your colleagues are still talking about it with their patients. It will validate and build the myopia-specific part of the practice and show the patients not involved in myopia management that your practice is cutting edge. “Even though we couldn’t control your myopia, Mrs. Patient, now if your kids follow your genetics, we have an option…”
The Power of Education
Sadly, many optometrists don’t consider myopia a big deal. Therefore, they will never educate their patients, making it all the more foreign a concept when bringing it up among the pediatric population. Simply mentioning myopia management to your regular patients validates it for your colleagues who offer the option.
Optometry has such an amazing opportunity to embrace myopia management. The gift of being able to slow, or even stop, a child’s myopic status is powerful to the patient and the parent, and they will tell their friends. The world is becoming more myopic, and we have a duty to reduce the complications that will follow those increasing numbers of longer eyes. Luckily, we have the tools for prevention, but we have to get parents and patients educated to use them. Providing state-of-the-art treatment for myopic children equals good things for children and our practice.

Katherine Schuetz, OD, is a private practitioner in Carmel, Ind., where she is a full-time clinician, splitting time between seeing pediatric patients at a primary care pediatric practice, Little Eyes, and teens through adults at RevolutionEYES. She is a Brilliant Futures panelist for CooperVision.
References
- Flitcroft DI. The complex interactions of retinal, optical, and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012; 31: 622–660.
- Brennan NA, Cheng X, Toubouti Y, Bullimore MA. Influence of Age and Race on Axial Elongation in Myopic Children. Optom Vis Sci 2018;95: E-abstract 180072.
- Tetsuya Ikeda, Kimiya Shimizu, Akihito Igarashi, Sumie Kasahara, Kazutaka Kamiya, “Twelve-Year Follow-Up of Laser In Situ Keratomileusis for Moderate to High Myopia”, BioMed Research International, vol. 2017, Article ID 9391436, 7 pages, 2017.
- Bullimore, Mark A. MCOptom, PhD, FAAO; Brennan, Noel A. MScOptom, PhD, FAAO2 Myopia Control: Why Each Diopter Matters, Optometry and Vision Science: June 2019 – Volume 96 – Issue 6 – p 463-465













