sponsored content
November 15, 2021
By Craig Brawley, OD, FAAO; Kevin Chan, OD, MS, FAAO; Millicent Knight, OD, FAAO, FAARM, FNAP; Pamela A. Lowe, OD, FAAO, Dipl. ABO; Moshe Mendelson, OD, FIAO; Yi Pang, MD, OD, PhD, FAAO
Although myopia-related eye diseases such as retinal detachment, cataracts, glaucoma, and macular degeneration occur typically in patients over 40 years old, these conditions can still happen in children and young adults.

A great deal of myopia management focuses on treatments that start during childhood to prevent future complications, such as retinal detachment, glaucoma, cataracts, or myopic maculopathy. But what happens to patients when their high myopia goes untreated?
Members from Essilor’s Myopia Task Force broke down cases from their real-life experiences to highlight the significant risks that are associated with high myopia. In each instance, a patient has developed a serious condition as a result of their untreated, high myopia. In some cases, it takes several years for those issues to develop, and in others, the effects occurred much sooner.
The goal is to spread awareness about the dangers of high myopia and ultimately reinforce the benefits associated with implementing myopia management treatment during early childhood.
Retinal Detachment Due to High Myopia
Craig Brawley, OD, FAAO; Vision Care Consultants, St. Louis, MO
- 50-year-old white female
- OD -7.25-1.25×008, OS -7.25-2.00×172.
- Med Hx: High Cholesterol, HTN, Hypothyroidism, Stomach Ulcers, Seasonal Allergies
- Meds: Atorvastatin, Cyclobenzaprine, Levothyroxine Sodium, Lisinopril
- Allg: PCN, polymyxin B
- No tobacco or drugs, minimal alcohol
- History of lattice degeneration related to her myopia. She called our office complaining of seeing a black spot in her vision that was becoming more of a curtain.
- Entering acuity in the right eye was 20/250. Upon examination, it was discovered that she had a partial macula off retinal detachment in her right eye. She was referred to a retinal specialist for treatment.
- Her best corrected vision is now 20/80 in the right eye. She has been prophylactically treated with laser retinopexy in the left eye where her vision currently is correctable to 20/20. She had a vitrectomy, laser, and buckle to repair RD, followed by cataract extraction and implantation.
- Final rx OD: -2.25-0.50×021 to 20/80
- She is currently wearing a Duette CL on her left eye for maximal vision.
Myopia-Related Retinal Manifestations
Kevin Chan, OD, MS, FAAO; Senior Clinical Director, Treehouse Eyes
- 15-year-old Indian male
- First onset of myopia at age 5
- Previous glasses Rx ~6 diopters “with some astigmatism as well”
- Glasses full-time wear
- Parents (both myopic) had no idea that ‘nearsightedness can be controlled’ yet also concerned about the rapid progression (~1 diopter per year)
- 2019 – Referred by ECP for an initial consultation for myopia management in my office
- Entrance aided VA (habitual glasses):
- OD -7.25 -1.00 x011 20/30-2
- OS -6.75 -1.50 x164 20/25-2
- Pre-treatment cycloplegic Rx (2019):
- OD -7.25 -0.50 x002 20/25-2
- OS -7.00 -1.00 x161 20/20-3
- Optic nerve cup-to-disc (C/D) ratio:
- OD 0.4/0.4
- OS 0.5/0.5
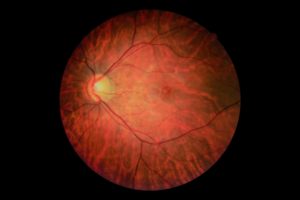
- Retinal appearance:
- Extensive peripapillary atrophy with disc tilting
- Peripapillary retinal pigment epithelium (RPE) ‘mottling’ → likely more susceptible to further deterioration → myopic maculopathy (MMD)
- More prominent sub-RPE/choroidal vasculature secondary to thinning retinal tissue as a result of myopia-related axial length elongation
- Extensive white-without-pressure (WsP) in 360-degree periphery
- Yet no retinal hole, tear, or detachment noted
- Current treatment regimen:
- Soft daily disposable extended-depth-of-focus (EDOF) multifocal contact lenses
- Topical atropine 0.025% instillation
- If-no-treatment prognosis:
- Already-high myopia will likely progress and deteriorate further
- For every diopter of myopia progression, 67% increased risk of MMD
- Current treatment progress:
- NO CHANGE in refractive status since 2019
- < +0.1mm axial length variation per eye per year since 2019
- Helps mitigate further myopia progression and potential lifelong complications resulting from high myopia
 |
 |
The retinal images from Dr. Chan’s patient.
A Family Affair Case Study (treatment initially provided two decades ago without resources available today for MM)
Millicent Knight, OD, FAAO, FAARM, FNAP
- Father, age 43, Asian, no systemic conditions
- Rx OD -8.25-3.50 x 005; OS -7.00-3.25 x 172, .4/.4 cups, no holes/tears, IOP 17/17 mm Hg
- Mother, age 35, Asian, no systemic conditions
- Rx -2.50 Sph OU, .2/.2 cups, no holes or tears, IOP 16/16 mm Hg
- Daughter, age 8, Asian, no systemic conditions
- Rx -1.00-.50 x 175; OS -1.50-.50 x 180 .3/.3 cups, (initial visit no internal/mother)
- Son, age 7, Asian, no systemic conditions
- Rx OD -4.50-.50 x 005; OS -4.00-1.00 x175, .2/.2 cups, intact retina *note 4’11’’ at initial visit (baseline)
- Son: Parents requested OrthoK for the son (their PedsOMD was not a proponent). Discussed Rx was now higher than I would usually fit with this modality. Parents were persistent with concerns of quality of life for their son. They declined treatment for their daughter. Patient (son) was fit with OrthoK at age 9 with close monitoring.
- Rx had increased: OD -7.50-1.00 x 180 OS -7.00-.75 x 175 20/20-1 OU
- Lenses worn successfully for over two years.
- Rx: OD -4.62-1.25 x 005, OS -4.00-2.87 x 161. Stable a few years.
- Patient presented with a small corneal ulcer OS end of year two.
- Dx: Chronic seasonal allergies, and vigorous eye rubbing. Lenses removed and treatment provided.
- Patient was non-compliant with OrthoK prior to the ulcer. Patient was also being seen by an OMD, who did not encourage OrthoK, and persuaded the patient’s parents to stop his treatment. He returned for glasses and soft CLs for myopia and astigmatism.
- I provided care for this patient from age 7 until age 21, when he graduated from college.
- Final Rx: OD-9.00-2.75 x 010 OS -8.50-3.00 x 165 20/20 OU c/d .3/.3 IOP 17/17 mm Hg
- Height ~6’4’’ by age 21
- Father: This patient was concerned about progressive myopia and requested OrthoK for his son at a time in the U.S. when it was not as common ~2002. Chief concern, not wanting his son to progress to his level of myopia.
- 7 years from initial visit: diagnosed with low tension glaucoma, co-managed with OMD
- 9 years from initial visit: significant vitreal floaters, and signs of MMD OS>OD
- 11 years from initial visit: mild cataracts, and progressing glaucoma (non-compliance with eyedrops)
- 12 years from initial visit: glaucoma and cataract surgeries
- Patient’s history puts him at a very high risk for retinal detachment. Last seen: age 53
- Final BVA OD 20/25, OS 20/40 (GLC advanced)
- Earlier intervention for both father and son, in particular, as well as tighter compliance statistically, would have provided for better outcomes.
Myopia Management: A Critical Part of Primary Eye Care
Pamela A. Lowe, OD, FAAO, Dipl. ABO; Professional Eye Care Center, Niles, IL
- Adult, Caucasian female
- -2.50 OD, -4.00 OS
- Patient developed glaucoma and required surgery in her 40s.
- Glaucoma progressed to require trabeculectomy surgery at age 50.
- Prior to surgery, patient had long enjoyed visual freedom with contact lenses; now, she’s unable to wear a contact lens in one eye due to issues with her filtering bleb.
- Patient’s father: -6.50OD, -7.00OS
- also a long-time contact lens wearer
- Developed early-onset cataracts in his 50s and subsequent retinal detachment.
- Both father and daughter suffered visual loss and complications that dramatically affected their quality of life.
In our role as primary eye care providers, it is our obligation to educate our at-risk myopic patients on strategies to prevent or delay onset and, when appropriate, treat as early as possible. We now know slowing myopic progression by 1 diopter reduces the risk of open-angle glaucoma by 20%, myopic maculopathy by 40%, and the risk of visual impairment (BCVA 20/40 or worse) by 20%, along with saving between 0.5 to 1.0 year of visual impairment.1 It is the primary care optometrist’s duty to manage patients with the “end in mind” and start implementing practice protocols to give our patients a lifetime of quality vision.
Glaucoma Due to High Myopia
Moshe Mendelson, OD, FIAO; Silicon Valley Eye Physicians, Sunnyvale, CA.
- 47-year-old male
- First seen in 2012
- OD –6.00 VA: 20/20 OS –6.00 -1.00 x 165 VA 20/20
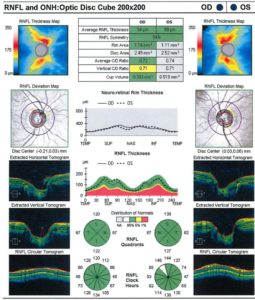
- CD: OD 0.4, OS: 0.5, IOP OD 15, OS 16
- Pachymetry OD 549 OS 559
- OCT – Normal findings
- VF: Full
- Continuous surveillance during annual eye exams from 2012 through 2018 including yearly IOP, OCT, and perimetry exams yielded normal findings.
- Patient returned for a routine yearly exam January 2021, during which OCT demonstrated right eye sector RNFL thinning.
- Comparison of 2021 OCT to 2012 OCT and perimetry demonstrate two adjacent 6 and 7 o’clock right eye RNFL thinning and a corresponding superior nasal visual field defect.
This is a case that supports the evidence described in the Blue Mountains Eye Study,2 which found that myopic eyes at the level of -3.00D to -6.00D are 3.3x more likely to develop glaucomatous damage and progressive visual field loss.
 |
 |
On the left is the data and imaging from Dr. Mendelson’s patient in October 2012 compared to the results in January 2021.
Struggles of Treating Young High Myopes
Yi Pang, OD, PhD, Illinois College of Optometry
- 8-year-old Caucasian female
- OD: -8.00 – 3.00 x 180 OS: -7.50 – 3.00 x 180
- She came to the clinic for a comprehensive eye exam and was interested in contact lenses. Post-dilation fundus findings were normal.
- Mother and patient were educated about myopia management options and what we could do to slow the myopia progression. The patient’s mother expressed understanding about the options and opted for soft multifocal contact lenses. We ordered Biofinity toric multifocal lenses, and the patient’s fitting appointment was scheduled for the following month. The patient’s mother rescheduled the appointment and came back three months later for the fitting appointment, at which point she indicated that everything with her child was stable.
- VA with trial lenses was 20/50 OD, 20/25 OS. Right CL rotated to left 15o and left CL rotated to left 5o.
- Even with the rotation of OD CL, I expected the patient would be seeing better than 20/50.
- I then performed 90 D fundus exam on an undilated pupil. Patient cooperation with 90 D was poor with no clear view on the macula. Even though the patient had a dilated exam three months prior, I decided to do a dilated fundus exam. I asked the patient’s mother if there were any problems with her child’s vision or eyes. Mother said everything was fine. With dilated fundus exam, superior and superior temporal retinal detachment was identified OD. I then referred the patient to a retinal specialist for retinal detachment surgery.
- The patient’s mother then told me that her child had complained about feeling like she had something in her eye for about a week. The mother didn’t think it was a big deal and didn’t report it to me.
Take-home message: Myopia is an eye disease that we, as eye care practitioners, should manage actively. Every diopter of myopia progression matters; thus, we should start the communication with parents and patients about myopia management earlier and plant the seeds earlier.
Although myopia-related eye diseases such as retinal detachment, cataracts, glaucoma, and macular degeneration occur typically in patients over 40 years old, these conditions can still happen in children and young adults. When it occurs in children, it makes it more challenging because it is hard for children to articulate their vision symptoms and feelings, making chief complaints unreliable. This was the youngest patient I’ve seen with retinal detachment as a result of myopia complications. With young children, their complaints are very vague; all this patient could tell her mother was that it felt like something was in her eye. With adults, we get things that are more concrete — they can tell us when their vision is obstructed.
The second challenge point for this case is that the 8-year-old girl had just had a comprehensive eye exam with dilated fundus exam three months prior. An eye care practitioner could assume that a recent eye exam should be sufficient to rule out possible fundus abnormalities. For this case, the girl was the last patient in the clinic, and she was not happy when I informed her that a dilated exam was needed. I am glad that I did it.
Complications can happen to children, even though it can be harder to get an accurate description of symptoms. This only makes myopia care more critical and comprehensive eye care more critical.
Conclusion
As these case studies have made clear, the risks associated with high myopia are severe and affect patients of all ages. This information highlights the importance of starting patients with myopia management solutions from a young age, and ultimately, doing everything possible to reduce the risk of damaging long-term eye health.
This article is sponsored by Essilor.
References
1 Bullimore, Mark A. MCOptom, PhD, FAAO1*; Brennan, Noel A. MScOptom, PhD, FAAO2 Myopia Control: Why Each Diopter Matters, Optometry and Vision Science: June 2019 – Volume 96 – Issue 6 – p 463-465. doi: 10.1097/OPX.0000000000001367
2 Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999 Oct;106(10):2010-5. doi: 10.1016/s0161-6420(99)90416-5. PMID: 10519600.













