March 15, 2021
By Larry Baitch, OD, PhD, FAAO
Arkady Selenow, OD, FAAO, ABO
Nabin Joshi, PhD
Inna Samandarova, PharmD
“This part-time treatment approach to myopia progression will likely add more value by increasing compliance and by least affecting the activities of daily living.”
Kubota Vision in Seattle, Wash., is developing The Kubota Glass System, a novel technology aimed at reducing myopia progression.
Multiple animal studies strongly suggest peripheral hyperopic blur in the retina to be the chief driver of myopia progression, resulting in axial elongation of the eye. Both human and animal studies have shown that even short-term, full-field myopic defocus, where the rays of light are focused in front of the retina, can produce small but significant relative reductions of axial length, which might unlock the pathways for minimizing such elongation.
The optimal peripheral stimulus that would be the most effective to slow myopia progression is currently unknown. In addition, inter-subject and intraocular differences are difficult to address with existing technology. Most myopia control devices in both spectacle design and contact lens form that utilize the peripheral myopic defocus principle rely solely on multifocal refraction-based defocus techniques, thus yielding only dioptric control of the defocused light in a designated area of the visual field.
How the System Works
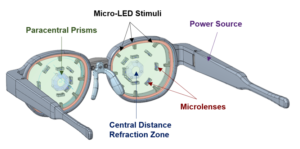
Figure 1: The Kubota Glass System has a self-contained battery that powers the micro-LED array to generate the peripheral defocus stimulus. The distance center segment contains the patient’s distance refractive error correction.
In contrast to the current approach, Kubota Vision has developed a novel, augmented reality-based optical system. The system has readily programmable control over important stimulus aspects for controlling eye growth, including the size, retinal location, luminance, chromaticity, duration of activation, and dioptric magnitude of the peripheral defocus stimulus. The Kubota Glass System allows for an opportunity to discover the optimal stimuli for controlling eye growth. Scientists at the Manhattan Vision Associates’ Institute for Vision Research (MVAIVR) have been working with Kubota Vision, performing a systematic series of studies to identify the most effective parameters and features for the device’s ergonomic functionality.
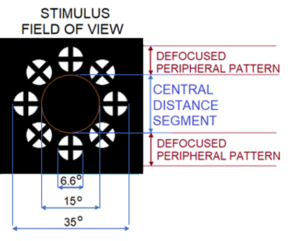
Figure 2: Layout of the defocused stimulus pattern employed in the Kubota glasses.
The Kubota Glass consists of white light-producing micro-LEDs. The patterned image is defocused by +3.50D micro-lenslets and is projected to the retinal periphery by the paracentral prisms, as shown in Figure 1. The device consists of a 15-degree diameter clear zone containing the distance refraction. This diameter was determined to be optimal for allowing normal eye movements, reading, and comprehension when the field is encompassed by a defocused periphery (Figure 2).

Figure 3: A representation of how the Kubota Glass System defocused light stimulus would appear to the wearer with its defocused pattern superimposed over the visual field.
The +3.50D peripheral defocus parameter was chosen as a result of earlier MVAIVR studies using full-field and peripherally applied Fresnel lenses. These studies showed decreased relative transient reduction in axial length. Preliminary data also suggest a correlated relative increase in subfoveal choroidal thickness, which if fully validated, agrees with studies by other investigators demonstrating transient increases of choroidal thickness. The image of the defocused pattern generated by the Kubota Glass with the visual field seen through the clear, focused light central aperture is shown in Figure 3.
The spatial content of the defocused image currently in the Kubota Glass was also selected based on the human prototype trials conducted by MVAIVR, with the cross stimulus producing a greater relative reduction in axial length compared to other configurations tested.
Mechanism of Action
Ophthalmic devices employing peripheral defocus methods engender a passive influence on the retina, and the parameters in those devices are not variable. In contrast, as an augmented reality-based optical system, the peripheral myopic defocus parameters of the Kubota Glass can be varied for maximum effectiveness and actively stimulate the retina.
For example, full annular field versus superior hemifield studies indicate that the efficacy of myopic defocus appears to vary with the region of the retina on which the defocus stimulus occurs. The Kubota Glass allows the bright, defocused light stimulus to be programmed to differentially affect specific regions of the retina as desired.
It has also been shown that myopic defocus, applied during certain times of the day, can potentiate and affect natural diurnal variations in the axial length and choroidal thickness. The Kubota Glass can manage daily treatment parameters, such as the timing and duration of the defocused light stimulus, which will allow for customized and personalized treatment for myopic progression based on individual diurnal variations.
Higher illumination of the outside environment is believed to be one reason for a lower risk of onset of myopia in children who spend more time outdoors. The Kubota Glass can control the luminosity of the peripheral defocus targets to mimic bright photopic conditions in the retinal periphery and to be brighter than the central field. In a study of young adults who received one hour of monocularly projected peripheral defocus, which was either 5, 10, or 20 times the brightness of the background, better results were obtained with the brightest luminance (20X ambient distance) of the peripheral projected stimuli. This finding highlights the importance of relative brightness of the defocused light in the retinal periphery and the importance of active peripheral stimulation. Chromaticity of the defocused light can be tailored, as well as the central distance aperture size for individual use. The Kubota Glass superimposes its projected defocused image onto the wearer’s visual field so that there is no distortion, as shown in Figure 2.
Prospective Use by Patients
Since the Kubota Glass System can vary the parameters of stimulus luminance, contrast, spectral content, and degree of peripheral defocus, a young patient at risk of future myopia progression would be prescribed to use the device for approximately one and a half to three hours per day corresponding to the typical cycle of diurnally fluctuating axial length (Figure 3). The patient can wear the Kubota Glass while performing normal daily activities such as classroom work, watching TV, or playing video games. The Kubota Glass System would be turned off or not worn during the downward trajectory of the normal, diurnal axial length curve (Figure 4) to facilitate a natural drop in axial length each day. This part-time treatment approach to myopia progression will likely add more value by increasing compliance and by least affecting the activities of daily living.
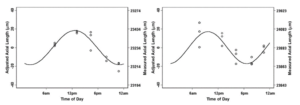
Figure 4: Data shown from two subjects (from Stone et al., 2004). Axial length data has been fit with sinusoids, showing the diurnal cycle.

Figure 5: E-Case charges KubotaGlass and can be used by ECPs to program its operation; E-Case also monitors daily compliance, that is the number of hours the device was actually worn by the patient.
In preliminary human studies, the Kubota Glass was well tolerated by wearers. It was reported as non-disruptive to vision even at the highest luminance intensity, based on a validated questionnaire. The Kubota Glass frame has been designed in collaboration with a leading custom frame designer (Vista Eyewear SRL, Belluno, Italy). MVAIVR is currently conducting multiple handling and wearability studies with the device. The Kubota Glass System will include a case that charges the device and maintains an accurate log of treatment compliance for review by the doctor and/or parents (Figure 5).
Longitudinal studies are now being performed on a Kubota Glass prototype on a pediatric cohort to determine the long-term effectiveness and, ultimately, the sustainability of this myopia control technology.
Larry Baitch, OD, PhD, FAAO, is Professor and Associate Dean for Research with MCPHS University School of Optometry, Worcester, Mass., and Arkady Selenow, OD, FAAO, ABO, Nabin Joshi, PhD, and Inna Samandarova, PharmD, are with Manhattan Vision Associates Institute for Vision Research (MVAIVR), New York, N.Y. Dr. Baitch is a paid consultant to MVAIVR, and Drs. Selenow, Joshi, and Samandarova are employees of MVAIVR.
References
- Chamberlain P, P.-d.-M. S. (2019). A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci, 96, 556–567.
- Edwards MH, L. R. (2002). The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci., 43, 2852–8.
- Hoseini-Yazdi H, V. S. (2019). Regional alterations in human choroidal thickness in response to short-term monocular hemifield myopic defocus. Ophthalmic Physiol Opt.
- Kubota R, Joshi NR, Samandarova I, Oliva M, Selenow A, Gupta A, Ali S, Ciuffreda K. (2020). Assessment of Visual Performance as a Function of Clear Central Aperture Diameter with a Defocused Periphery: Application to Myopia Control.
- Kubota R, Joshi NR, Samandarova I, Oliva M, Selenow A, Gupta A, Ali S, Ciuffreda K. Visual Performance as a Function of Clear Central Aperture Diameter with a Defocused Myopic Periphery. Optometry & Vision Science, in press.
- Kubota R, Joshi NR, Samandarova I, Oliva M, Selenow A, Gupta A, Ali S. Effect of short-term peripheral myopic defocus on ocular biometrics using Fresnel “press-on” lenses in human subjects. Abstract accepted for Meeting of the Association for Research in Vision and Ophthalmology (ARVO), 2021.
- Smith EL III (2011) The Charles F. Prentice award lecture 2010: a case for peripheral optical treatment strategies for myopia. Optometry and Vision Science. 88, 1029.
- Stone RA, Q. G. (2004). Diurnal axial length fluctuations in human eyes. Invest Ophthalmol Vis Sci., 45(1), 63-70.













