December 1, 2020
By Divya Jagadeesh, BOpt, MPhil, PhD
No level of myopia is considered safe, and any increase in myopia is said to increase the risk of developing complications.1 Thus, the goal of myopia management should not only focus on correcting the refractive error to restore vision but should address any risk of progression and/or complications.
Therefore, when examining an individual with myopia, in addition to evaluating refractive error and axial length, there is a need for additional assessments that aid in estimating the risk of progression and evaluating the health of the eye.
Estimating the Risk of Progression
Myopia progression rates may vary depending on several factors, including age, gender, ethnicity, genetic/parental, and environmental factors. For example, a young myopic child of Asian ethnicity and myopic parents is likely to be at risk of faster progression; such an individual may require a myopia management strategy that has been proven to provide a significant level of control.2,3 Table 1 lists the various risk factors found associated with myopia progression. Considering these risk factors in association with refractive error and/or axial length assessment may indicate if an individual is at increased risk of progression.
Table 1: Risk Factors Associated with Myopia Progression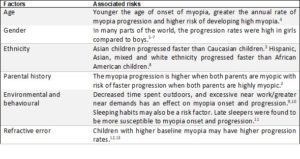
Simple e-tools also help practitioners convey and educate individuals and their families on the risk of progression. These include the BHVI Myopia Calculator, Myopia Care, and Myopia Profile.
More recently, we have seen an effort to integrate the clinical measurements of refractive error and axial length with the demographic, parental, and environmental factors to provide a comprehensive risk assessment. For example, the Oculus Myopia Master enables the measurement of corneal curvature, refractive error, and axial length in a single instrument. Additionally, it provides an estimation of the risk of future progression utilizing percentile charts for axial length dimensions, demographic, parental, and environmental risk factors. (The Myopia Master is not yet FDA approved.)
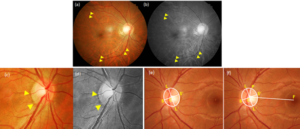 Figure: (a) & (b) Tessellated fundus appearance as denoted by yellow pointers in (a) Color fundus image (b) Gray scale fundus image of the same eye. Temporal crescent as denoted by yellow pointers in (c) Color fundus image (d) Gray scale fundus image of the same eye. Optic disc ovality and rotation – ovality index measured as the ratio of the longest (LL’) and shortest (SS’) diameter. (b): rotation ; deviation of the long diameter (LL’) of the optic disc from PC. The reference line (FC), 90° is a horizontal line connecting the fovea (F) and the centroid of the optic disc (C) and PC is the perpendicular. Oval discs had ovality index ratios exceeding 1.30. Rotated discs – was >15°.
Figure: (a) & (b) Tessellated fundus appearance as denoted by yellow pointers in (a) Color fundus image (b) Gray scale fundus image of the same eye. Temporal crescent as denoted by yellow pointers in (c) Color fundus image (d) Gray scale fundus image of the same eye. Optic disc ovality and rotation – ovality index measured as the ratio of the longest (LL’) and shortest (SS’) diameter. (b): rotation ; deviation of the long diameter (LL’) of the optic disc from PC. The reference line (FC), 90° is a horizontal line connecting the fovea (F) and the centroid of the optic disc (C) and PC is the perpendicular. Oval discs had ovality index ratios exceeding 1.30. Rotated discs – was >15°.
In addition to cataloging the demographic and environmental-related risk factors, an examination of the eye is useful as the presence of certain posterior segment features/signs is linked with progression.
- Appearance of tessellations (tigroid appearance) in the fundus may be associated with myopia progression.14,15 Of the myopic children who presented with tessellated fundus appearance, 76 percent progressed over a 10-year period.16
- Optic nerve ovality and rotation was associated with myopia progression.17
- Due to its strong association with myopic refractive error and frequency of occurrence even in young myopic eyes,18 myopic conus is of interest. Myopic conus, usually a temporal crescent (sometimes inferior), may increase in size in direct proportion with axial length change.19
Evaluation of the Health of the Eye
A thorough and comprehensive examination of the eye helps appraise the current and future risk of eye disease. Although degenerative changes such as chorioretinal atrophy are more commonly observed in mature eyes, there are many posterior segment conditions/changes such as lattice degeneration and retinal breaks observed in young myopes and, in some instances, may require immediate attention. Table 2 catalogs the posterior segment signs observed in myopic eyes.
Managing Myopia Progression
If determined that the eye is at risk of progression, several interventions exist from which a strategy appropriate for the individual may be chosen. These range from spectacle lenses (peripheral defocus, executive bifocal, defocus inducing multiple segments), contact lenses (dual focus, reduction of peripheral defocus and/or inducing myopic defocus, extended depth of focus, orthokeratology), pharmaceutical (atropine), and environmental strategies (increased outdoor time).21
Table 2: Features/Signs Linked with the Progression of Myopia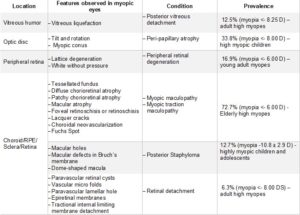
If the myopic eye exhibits one or more signs described in Table 2, depending on the feature/sign, the practitioner may a) record and monitor for changes at future visits (for example, white without pressure); b) monitor more closely (for example, lattice degeneration in a moderately myopic eye); or c) refer to a specialist for treatment (for example, retinal detachment or retinal break). All individuals with myopia and/or their caregivers/families should be educated on the possible risk of progression and complications associated with myopia, the importance of myopia management, and any unwanted effects associated with such treatments.
 Divya Jagadeesh, BOpt, MPhil, PhD, is a research fellow with BHVI. She acknowledges the support of Professor Padmaja Sankaridurg for the editing and revision of this clinical article.
Divya Jagadeesh, BOpt, MPhil, PhD, is a research fellow with BHVI. She acknowledges the support of Professor Padmaja Sankaridurg for the editing and revision of this clinical article.
References,
1 Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 2012; 31: 622-660.
2 Saw SM, Nieto FJ, Katz J et al. Familial clustering and myopia progression in Singapore school children. Ophthalmic Epidemiol 2001; 8: 227-236.
3 Donovan LA, Sankaridurg P, Ho A et al. Rates of Myopia Progression in Children. Invest Ophth Vis Sci 2010; 51.
4 Sankaridurg P, Holden BA, Donovan LA et al. An Annual Rate of Myopic Progression Model for Asian children. Invest Ophth Vis Sci 2014; 55.
5 Saw SM, Tong L, Chua WH et al. Incidence and progression of myopia in Singaporean school children. Invest Ophth Vis Sci 2005; 46: 51-57.
6 Loman J, Quinn GE, Kamoun L et al. Darkness and near work: myopia and its progression in third-year law students. Ophthalmology 2002; 109: 1032-1038.
7 Donovan L, Sankaridurg P, Ho A et al. Myopia Progression Rates in Urban Children Wearing Single-Vision Spectacles. Optometry Vision Sci 2012; 89: 27-32.
8 Hyman L, Gwiazda J, Hussein M et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol-Chic 2005; 123: 977-987.
9 Wong CW, Tsai A, Jonas JB et al. Digital Screen Time During COVID-19 Pandemic: Risk for a Further Myopia Boom? Am J Ophthalmol 2020.
10 Kinge B, Midelfart A, Jacobsen G et al. The influence of near-work on development of myopia among university students. A three-year longitudinal study among engineering students in Norway. Acta Ophthalmol Scan 2000; 78: 26-29.
11 Liu XN, Naduvilath TJ, Wang JJ et al. Sleeping late is a risk factor for myopia development amongst school-aged children in China. Sci Rep-Uk 2020; 10.
12 Saw SM, Nieto FJ, Katz J et al. Factors related to the progression of myopia in Singaporean children. Optometry Vision Sci 2000; 77: 549-554.
13 Chua SYL, Sabanayagam C, Cheung YB et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthal Physl Opt 2016; 36: 388-394.
14 Yan YN, Wang YX, Yang Y et al. Long-term Progression and Risk Factors of Fundus Tessellation in the Beijing Eye Study. Sci Rep-Uk 2018; 8.
15 Jagadeesh D, Philip K, Naduvilath TJ et al. Tessellated fundus appearance and its association with myopic refractive error. Clin Exp Optom 2018.
16 Wong YL, Sabanayagam C, Ding Y et al. Prevalence, Risk Factors, and Impact of Myopic Macular Degeneration on Visual Impairment and Functioning Among Adults in Singapore. Invest Ophth Vis Sci 2018; 59: 4603-4613.
17 Kim M, Choung HK, Lee KM et al. Longitudinal Changes of Optic Nerve Head and Peripapillary Structure during Childhood Myopia Progression on OCT Boramae Myopia Cohort Study Report 1. Ophthalmology 2018; 125: 1215-1223.
18 Kobayashi K, Ohno-Matsui K, Kojima A et al. Fundus characteristics of high myopia in children. Japanese Journal of Ophthalmology 2005; 49: 306-311.
19 Moon Y, Lim HT. Relationship between peripapillary atrophy and myopia progression in the eyes of young school children. Eye 2020.
20 Jagadeesh D, Philip K, Fedtke C et al. Posterior segment conditions associated with myopia and high myopia. Clin Exp Optom 2020; 103: 756-765.
21 Wildsoet CF, Chia A, Cho P et al. IMI – Interventions for Controlling Myopia Onset and Progression Report (vol 60, pg M106, 2019). Invest Ophth Vis Sci 2019; 60: 1768-1768.













