sponsored content
December 15, 2023
By Tina Goodhew, OD, with commentary by Cristina Schnider OD, MBA, FAAO
 Though not yet available in the United States, several spectacle lens designs with demonstrated efficacy for myopia control are currently accessible to Canadian practitioners. I had the unique opportunity to compare myopia control spectacles with two disparate designs and modes of action in a pair of myopic 8-year-old identical twin females.
Though not yet available in the United States, several spectacle lens designs with demonstrated efficacy for myopia control are currently accessible to Canadian practitioners. I had the unique opportunity to compare myopia control spectacles with two disparate designs and modes of action in a pair of myopic 8-year-old identical twin females.
The twins had shown progressive increases in myopia prior to a September 2021 visit to the office, and because identical twins presented a rare opportunity to evaluate two spectacle designs with a built-in mini “control group,” each twin was prescribed a different design. The parents agreed given that both designs had been shown to be highly effective at slowing myopia progression in published studies. One design featured diffusion optics technology to create contrast modulation via a proprietary pattern of thousands of microscopic scattering dots from edge to edge with a clear central zone (DOT), and the other used peripheral defocus technology with the defocus incorporated around a clear central zone.
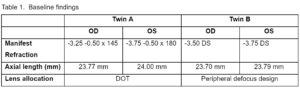
Baseline refraction, axial length, and randomly assigned lens design allocation for each twin are shown in Table 1.
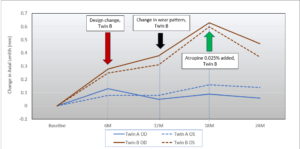
The glasses in the assigned design were dispensed to each twin with instructions to wear them at all times. At the one-month follow-up visit, both twins were wearing their glasses consistently with no complaints about appearance or functionality for either design. At the six-month post-dispensing visit, however, Twin B had progressed at approximately twice the rate of Twin A for both axial length (AL) and spherical equivalent refraction (SER). Due to the large differences in rates of progression and a request from the mother, Twin B was switched to the contrast management (DOT) design. As shown in Figure 1, the change in design initially altered the rate of progression of both AL and SER for Twin B over the second six-month period, as evidenced by the flatter trajectories between six and 12 months. Progression rates were more in line with that of Twin A wearing the same design.
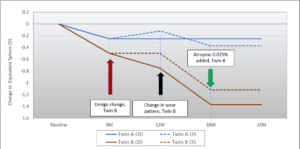
Figure 1. Change in (i) axial length and (ii) spherical equivalent refraction over time with identical twins fit with two unique spectacle lens designs for myopia control. Twin A wore a contrast management design (DOT) for the entire 24 months of follow-up. Twin B wore a peripheral defocus design for the first six months followed by the contrast management design (DOT) for the last 18 months. Non-compliance with a full-time wear schedule was reported between 12 to 18 months for twin B. (click to enlarge figures)
Interestingly, at the 18-month visit, Twin B had again progressed at a much faster rate than Twin A despite wearing the same design spectacle lens for the prior year. The mother reported that Twin B had been resisting wearing her glasses since the last visit. The mother declined the option of contact lenses, so we opted for an updated frame, and I added 0.025% atropine to be instilled before bed in hopes of gaining better control of myopia for Twin B. Happily, at the 24-month visit, both twins had stabilized, with Twin B actually showing a reduction in AL and a stable SER from 18 months. The mother requested that atropine be added to the regimen for Twin A in order to do everything possible to slow progression, though I felt it was optional for that case.
Afterword by Dr. Cristina Schnider
In this case with identical twins providing a unique situation for controlling variables, we saw a clear difference in progression of AL as well as SER with the two different spectacle lens designs. But when looking at myopia progression in young patients on a day-to-day basis, it is important to realize that progression varies with age, and therefore we need to know what is considered normal for a given age to determine if, when, and how to intervene.
Because of the associated pathologies throughout life resulting from axial elongation, axial length is the more critical parameter to monitor. An excellent paper by Chamberlain and colleagues provides some useful perspectives on what constitutes “normal” progression.1 Using the Orinda Longitudinal Study of Myopia (OLSM), their model predicts axial elongation of 0.15mm and 0.13mm for emmetropes and 0.25mm and 0.28mm for myopes, respectively, for the age range of our twins (8 to 9 years of age during this course of treatment).
For the first six-month wear period in this case study, the contrast management design (DOT) yielded rates of axial elongation of ~ 0.08mm/year, which is consistent with the modeled values for emmetropes. However, the peripheral defocus design results (≥ 0.25mm in six months) were as high or higher than the modeled values of elongation seen in untreated myopic subjects. Switching designs in Twin B slowed the rate during six months of compliant (full-time) wear, faltered when compliance dropped off in the next six months, and stabilized with the addition of atropine and some more up-to-date frames.
In summary, this case provides some key insights into myopia management:
- Despite potential concerns over the visibility of the microdot pattern on the DOT spectacle lenses, neither parents nor patients made any mention of an issue related to the lens appearance. It’s important not to introduce negative preconceptions when discussing options.
- For these twins, the contrast management design (DOT) provided better control of axial length and refractive changes than the peripheral defocus design, at least when worn consistently. This is a very small sample, however, so avoid jumping to conclusions based on this case report.
- Compliance with a full-time wear schedule had an apparent impact on efficacy. This has been reported elsewhere as well. It is imperative that children and parents understand the importance of full-time wear for all activities to achieve the full effect of the therapy.
This article is sponsored by SightGlass Vision.
 |
Tina Goodhew, OD, is a graduate of the University of Waterloo School of Optometry and Vision Science. She is active in service to the profession of optometry. Dr. Goodhew served on the Board of Directors for the BC College of Optometrists in the early 2000s. From 2010 through 2016, she was a director for Eye Recommend, a group responsible for helping chart the course of optometry in Canada. She has given numerous talks to colleagues and community groups and currently serves as a key opinion leader for Alcon, CooperVision, Bausch & Lomb, and Sightly.
|
 |
Cristina Schnider, OD, MBA, FAAO, is the sole proprietor of C Schnider Insights, providing insights, education, and editorial services in the areas of cornea, contact lenses, and refractive technologies. She spent 14 years in education and research in the U.S. and Australia before joining industry, where she continued pursuing those passions for another 20 years. She now enjoys her consulting work, splitting time between the Pacific Northwest of the U.S., the southern tip of Australia (Tasmania), and Japan. |
Reference
- Chamberlain P, Lazon de la Jara P, Arumugam B, Bullimore MA. Axial length targets for myopia control. Ophthalmic and Physiological Optics. 2021 May;41(3):523-31.