sponsored content
February 1, 2023

Many of us have experienced watching a sports figure who, at a particular time, is at their most precise and can do no wrong. This is often described as being “in the zone.” One of the most talked about recent innovations in orthokeratology design is the development of varied optic zone sizes, particularly smaller optic zones for myopia management. Randy Kojima, FAAO, FBCLA, FSLS, FIAOMC, has been “in the zone” in terms of OrthoK design for decades and is undoubtedly considered an expert in this area. Here, Bruce Morgan, OD, Art Optical’s Executive Director of Research and Clinical Support, discusses OrthoK zone sizes with Kojima, Clinical Research and Development Director for Precision Technology and a partner in the KATT Design Group.
Bruce Morgan, OD: How did the idea of creating different optic zone sizes for OrthoK lenses come about?
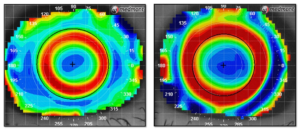
Randy Kojima, FAAO, FBCLA, FSLS, FIAOMC: That’s a great question. I’m not sure there is a published reference to draw from here. I can say the first time I heard about the idea was from Professor Patrick Caroline at Pacific University. He suggested we might be able to alter the position of the red ring we observe on the tangential topography analysis that is present following OrthoK treatment. Could we affect the position of the red ring if we were to move the reservoir position? Previously at Pacific U, we had observed that the magnitude of paracentral changes appeared correlated with the Rx change. The lower the Rx change, the larger the treatment zone and the lower the paracentral tangential steepening. Conversely, the higher the Rx change, the smaller the treatment zone and the greater the curvature changes in the red ring. Similarly, could the deepest part of the optical zone and reverse curve junction control the size of the treatment zone or the blue area of central flattening we see on the axial topography map?
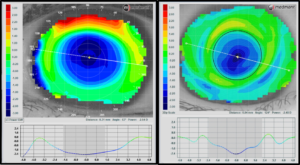
Figure 2: Comparison of Treatment Zone Size Using Large vs. Small Optic Zones (Axial Treatment Profile)
Dr. Morgan: What actually happens to the lens in terms of the other parameters outside the optic zone?
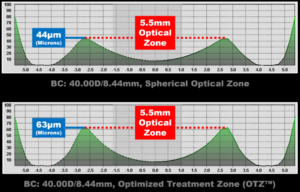
Kojima: When altering the optical zone size while leaving the lens diameter the same, something must change in compensation. Typically, either the reverse curve or alignment zone must increase in size to compensate. In the Moonlens, the alignment zone maintains the same width regardless of optical zone size. However, the reverse curve will widen with decreasing optical zone diameters.
It is hoped that the wider reservoir will have a positive effect on the pull force applied to the peripheral cornea. In other words, will the wider tear reservoir increase the surface area of paracentral steepening and therefore create a larger surface area of defocus for improved myopia control?
Dr. Morgan: Do different optic zone sizes affect the all-important tear film profile under the lens?
Kojima: The principal contribution to tear layer changes between optical zones is the position of the deepest point of the tear reservoir. That is to say, the larger the optical zone, the farther away from the central cornea the highest tear layer thickness will be. Alternatively, the smaller the optical zone, the closer to the central cornea, the deepest point of the reservoir will be. Using different optical zone sizes provides the clinician with control over the power profile created on the anterior corneal surface. This means we can better control the distribution of power that enters the pupil. Do we want the power profile to create less spherical aberration or more spherical aberration? For adult or adolescent eyes, we want very different outcomes.
The Moonlens also uses unique construction when it comes to building the depth of the reservoir and not just its position. While the smaller optical zones move the suction force farther in or closer to the corneal apex, the lens also manipulates the height of the reservoir to maximize the tear pressure force in myopia management cases and high minus treatment. Using both a smaller optical zone and optimized tear layer depth, the Moonlens approaches OrthoK treatment in a revolutionary and truly customized manner.
Dr. Morgan: What specific advantages do smaller optic zones have on managing myopia?
Kojima: Smaller optical zones have been shown to slow down eye growth in children even more than conventional 6 mm OZ designs. The Guo study from Hong Kong Polytechnic1 presented findings comparing a 5.0 mm to a 6.0 mm optical zone in children over a two-year period. The smaller OZ had substantially less axial elongation and slowed eye growth by an astounding 76% compared to conventional glasses-wearing control groups.
But the smaller optical zone isn’t only beneficial in myopia control applications. Moving the reservoir position closer also makes it possible to achieve a higher magnitude of effect. In other words, higher sphere and cylinder corrections are possible when the hydraulic force is concentrated over a smaller surface area. So, smaller optical zones have multiple benefits in OrthoK.
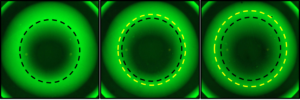
Figure 4: (Left: 5.0 mm; Middle: 5.5 mm; Right: 6.0 mm) Deepest/Most Powerful Part of Return Zone Closer to Center of Treatment with Smaller Optic Zone Sizes
Dr. Morgan: How do we know we have provided the optimal optic zone size for a particular patient?
Kojima: Unfortunately, we don’t know until we start OrthoK treatment. Before starting the process, we have yet to determine a method or analysis to define what optics an individual patient requires. However, we do have a guideline. Adolescents benefit from a higher spherical aberration signal sent to the back of the eye. The higher the aberration sent to the retina, the less the eye grows. Conversely, the adult is much more sensitive to the aberrations and requires us to design the lenses to lessen the aberrations. Once treatment has commenced, it’s possible to determine the degree of spherical aberration created, and the patient’s visual response is an excellent measure of the effect. If either child or adult struggles with visual disturbance, we know the spherical aberration or blur signal is too strong. This can be reduced by going with a larger optical zone. In children, we attempt to maximize peripheral blur to create the largest myopia control signal possible. Then we monitor the patients over time to ensure that the signal is strong enough, as indicated by the axial length changes. But the topographer can measure the spherical aberration, treatment zone size, and peripheral steepening in the early days of treatment. The practitioner does not have to let the patient go for six months only to find out the eye continues to grow. We can measure the effects in the early days of treatment to determine if changes are needed.
The Moonlens calculator helps determine an optical zone size that will likely be ideal for the patient based on their age and Rx. This helps take some guesswork out of customized OrthoK lens construction.
Dr. Morgan: Are there potential other benefits related to varied optic zone sizes besides myopia management?
Kojima: Reducing the optical zone size means greater curvature changes are possible over a smaller surface area. It has been determined that OrthoK primarily affects one tissue layer of the cornea, the epithelium. If this is true, we have only so much tissue to work with, about 50 microns. To create a 1.00D myopic reduction involves a small change to the epithelial thickness. However, to create a 5.00D effect, a large change in shape and power must take place. Then, adding an astigmatic requirement means you need even more effect to the steep axis of the cornea, assuming the refractive cylinder is primarily corneal. It is easier to create these bigger shape changes over a smaller surface area of the cornea. Small optical zones provide the ability to manipulate central tissue, so higher curvature changes are possible and, therefore, higher reduction to sphere and cylinder correction.
Dr. Morgan: Is there a downside to using a smaller optical zone in OrthoK?
Kojima: As mentioned earlier, the smaller the optical zone, the smaller the resultant treatment area created on the anterior surface of the cornea. The smaller the treatment zone, the higher the spherical aberration signal. Every patient has a different threshold of how much aberration their visual system can manage. It is important to know that some patients may struggle with the blur created that most patients can manage. As with the fitting of multifocal contacts, the magnitude of the add power can have the effect of creating too much aberration, and we lose visual function rather than gain additional magnification. It is similar in OrthoK. We may need to increase the treatment area for some patients because the aberrations created are higher than a patient’s visual system can manage. This may happen for approximately 5-10% of patients. In such cases, we simply order the next larger optical zone size, which typically resolves the visual disturbance the patient might be experiencing.
References:
1 Guo B, Cheung SW, Kojima R, Cho P. Axial elongation over two years using small back optic zone diameter orthokeratology lenses; Poster: Vision by Design, Bellevue, WA, 9/2022.