November 1, 2022
By Krupa Philip, BOptom, PhD, Senior Research Scientist at BHVI
Although it is challenging to perform refractive error assessments in young children, it is rewarding when a successful outcome is achieved and the child and their parents/caregivers are satisfied with the outcome.
Given that all the indicators are for a rising prevalence of myopia,1 it is quite likely that practitioners will increasingly see children in their practices. Other common reasons for a young person to present at an eye care practice include conditions such as strabismus, amblyopia, astigmatism, and ocular allergies.
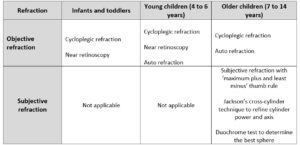
The purpose of refraction is to ensure that the eye’s refractive state is appropriately assessed and whether an optical correction is needed/adjusted to restore vision to its optimum. Eye care practitioners are quite familiar with the techniques to assess refractive error; they range from subjective refraction and retinoscopy to autorefraction and aberration techniques. These techniques, alone or in combination, provide a good assessment of the refractive state. However, many other factors influence the assessment and outcome when dealing with children. For example, in very young children, subjective refraction may be challenging due to difficulties with communication and/or responsiveness to instructions; they may also be inattentive or easily distracted. Additionally, based on this principle, there may be some variation in the refractive error measured with the various instruments/techniques. Furthermore, in young children, accommodation is active, but the response varies depending on age and refractive error. In very young children, and those with hyperopia, emmetropia, and low levels of hyperopia, there is over-accommodation to near targets (proximal accommodation). These may result in over-minusing and possibly a misdiagnosis of the refractive error.2 Even if appropriate procedures are adopted to relax accommodation, such as using plus lenses and/or use of a dark room, distance gazing, etc., it might be challenging to ensure that the accommodation is fully relaxed.
Given the above issues, conducting cycloplegic refraction in young children is common to ensure an accurate read of the refractive error status. According to IMI — Clinical Management Guidelines, cycloplegia can be achieved by instilling two drops of 1% cyclopentolate or 1% tropicamide drops five minutes apart and performing the objective refractive 30-45 minutes after the last drop instillation.3 Studies have shown that tropicamide is the preferred cycloplegic agent due to its rapid onset of action, shorter recovery time, and fewer side effects.4 To ensure that the eye is adequately cyclopleged, sufficient time should be allowed after the instillation of the last drop of cycloplegic. The eye care practitioner should confirm that pupils are fixed and dilated either with a slit lamp or with a torchlight.
After that, an objective refraction can be performed either with retinoscopy or autorefractor, followed by subjective refraction. Suppose there is no cycloplegia (also referred to as “dry” refraction). In that case, it is vital to relax accommodation via the use of fogging lenses, or have children view into the distance (do not use optotype targets, as the eye tries to focus and clear these images). In these situations, it is advisable to perform visual acuity tests and compare them against the non-cycloplegic refractive error assessments to determine if the assessment was appropriate. For example, suppose the visual acuity of the child is near normal, but their non-cycloplegic assessment reveals substantial myopia. In that case, it indicates that the eye was not sufficiently relaxed during their assessment.
Objective Refraction
Retinoscopy
When it comes to an objective technique for refractive error assessment, mastering retinoscopy is a valuable and essential skill for very young children, especially infants and toddlers. It is the most preferred since it requires the least amount of engagement/cooperation from the child and does not require other accessories or modifications to enable the measurement.5 It is recommended that an appropriate fogging technique is used.6 However, it has been reported that refraction under fogging is said to elicit more minus power or less plus power compared to refraction under cycloplegia in children.7
A) Near Retinoscopy or Mohindra Retinoscopy
In young children (infants and toddlers), it is ideal to perform near retinoscopy or Mohindra retinoscopy. While performing Mohindra retinoscopy or near retinoscopy, ensuring that the room is dark will facilitate that the child seated in their parent’s/caregiver’s lap will directly focus on the retinoscope light in front of them. The retinoscope should be held 50 cm away from the child while performing the retinoscopy, and loose lenses should be used to assess the refractive state. When finished, add +1.25D to the gross measurements.
B) Static or Distance Retinoscopy
In children aged 3 years or older, static retinoscopy could be performed with fogging lenses in place. It is important to encourage the child to relax their accommodation by looking into the distance and not at the retinoscope light.
Autorefraction
Autorefractors can measure refraction in children when they can be sufficiently engaged, comfortably positioned at the instrument, and follow instructions.5 Even though autorefractors employ built-in fogging mechanisms to control accommodation, conventional closed field autorefractors can induce accommodation due to the proximity of the instrument. Therefore, these may result in misdiagnosis, such as overestimating myopia or underestimating hyperopia.8 An alternative is the open-field autorefractor, with less likelihood of triggering proximal accommodation. For these reasons, where possible, it is essential to instill cycloplegic drops in children before performing autorefraction.
Subjective Refraction
When children are older (commonly 6 to 7 years or above) and can respond to instructions, subjective refraction can be performed. The subjective refraction should begin with maximum plus for hyperopic children and least minus for myopic children and reach the subjective endpoint using 0.25D increments or decrements. Since undercorrection is not useful in managing myopia, it is important to provide the refractive error that provides the best vision. A duochrome test can be performed monocularly or binocularly to check on the best vision sphere. While performing the duochrome test, if the letters/rings on the green side of the chart appear darker/clearer, increase by +0.25D steps and decrease by -0.25D steps if the letters/rings on the red side of the chart appear darker/clearer. The child needs to tell the clinician which side of the chart the letters appear “darker/clearer.” The endpoint of the test is when letters on both the red and green side of the chart appear equally dark/clear to the patient. Finally, a Jackson’s cross-cylinder technique can be used to fine-tune the cylinder power and axis for older children.
In summary, although it is challenging to perform refractive error assessments in young children, it is rewarding when a successful outcome is achieved and the child and their parents/caregivers are satisfied with the outcome. Because children adapt and learn rapidly, practitioners will find it easier to perform refraction at follow-up visits.
 |
Dr. Krupa Phillip has more than 10 years of experience in myopia management and holds post-doctoral qualifications as a senior research scientist working in refractive errors and myopia with Prof. Sankaridurg at BHVI. She has a particular interest in ocular aberrations and visual experience with various myopia management strategies. Dr. Phillip has published several articles and co-authored a book chapter on refractive error and eye health in Southeast Asia. Currently, she is managing clinical trials in general health. |
References
- Holden, B.A., et al., Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology, 2016. 123(5): p. 1036-42.
- Sankaridurg, P., et al., Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol, 2017. 95(7): p. e633-e640.
- Gifford, K.L., et al., IMI – Clinical Management Guidelines Report. Invest Ophthalmol Vis Sci, 2019. 60(3): p. M184-m203.
- Yazdani, N., et al., Comparison of cyclopentolate versus tropicamide cycloplegia: A systematic review and meta-analysis. J Optom, 2018. 11(3): p. 135-143.
- Kemper, A.R., et al., Comparison of monocular autorefraction to comprehensive eye examinations in preschool-aged and younger children. Arch Pediatr Adolesc Med, 2005. 159(5): p. 435-9.
- Jorge, J., et al., The influence of cycloplegia in objective refraction. Ophthalmic Physiol Opt, 2005. 25(4): p. 340-5.
- Hopkins, S., et al., Refraction in children: a comparison of two methods of accommodation control. Optom Vis Sci, 2012. 89(12): p. 1734-9.
- Choong, Y.F., A.H. Chen, and P.P. Goh, A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am J Ophthalmol, 2006. 142(1): p. 68-74.