Sponsored Content
August 17, 2020
By Daniel Press, OD, FCOVD
 As eye care professionals, when you see one patient with complications that can be associated with myopia, you have seen one too many patients with complications associated with myopia. The question at hand is related to the core purpose of providing myopia mitigation services in clinical practice. Patient communication is commonly cited as the most challenging aspect of providing specialty services, including myopia management. The effort that it takes educating patients and caregivers on the risks associated with higher levels of myopia, along with the treatment options, stresses our most valuable resource, time. Wouldn’t it be nice if the general public understood the risk factors associated with myopia, similarly to the universal understanding of the risk factors associated with smoking? There are a number of reasons why we are constantly spending time educating our patients and their guardians on the pathology associated with myopia. Here are three:
As eye care professionals, when you see one patient with complications that can be associated with myopia, you have seen one too many patients with complications associated with myopia. The question at hand is related to the core purpose of providing myopia mitigation services in clinical practice. Patient communication is commonly cited as the most challenging aspect of providing specialty services, including myopia management. The effort that it takes educating patients and caregivers on the risks associated with higher levels of myopia, along with the treatment options, stresses our most valuable resource, time. Wouldn’t it be nice if the general public understood the risk factors associated with myopia, similarly to the universal understanding of the risk factors associated with smoking? There are a number of reasons why we are constantly spending time educating our patients and their guardians on the pathology associated with myopia. Here are three:
Myopia is a term that is unfamiliar to the general population. Our profession historically used nearsightedness interchangeably with myopia. In our practice, myopia is used exclusively and explained as the medical term for nearsightedness, which encompasses more than the experience of blurred distance vision. Myopia is a complex condition that involves genetic and environmental influences that result in axial elongation and associated complications. Myopia is the preferable term. Considering it is estimated that 17 exposures are needed to learn a new word, it is not surprising that more of the population is not aware of the word itself as well as the concerns regarding myopia.
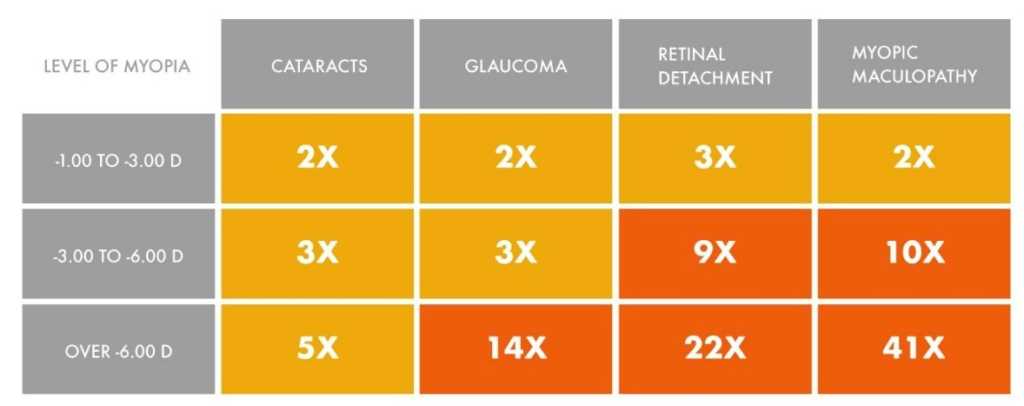 The overall incidence of pathology related to myopia is relatively small. A common reference used for the incidence of pathology related to myopia is from Prof. Ian Flitcroft’s 2012 paper, “The complex interactions of retinal, optical and environmental factors in myopia aetiology”1 and is summarized in this table:
The overall incidence of pathology related to myopia is relatively small. A common reference used for the incidence of pathology related to myopia is from Prof. Ian Flitcroft’s 2012 paper, “The complex interactions of retinal, optical and environmental factors in myopia aetiology”1 and is summarized in this table:
Evaluating the patient with reduced vision due to myopic maculopathy highly motivates us to limit myopic progression in childhood. Research by Fricke et al2 estimated that, globally, 10 million people had visual impairment in 2015, which represents a 0.13 percent incidence. Visual impairment was defined according to the World Health Organization as 6/18 (20/60 for Americans). While not clearly articulated in Fricke’s article, most studies report visual acuity on a monocular basis. How many of those patients reported in the article show functional deficits related to their visual impairment? Blindness was defined as 3/60 or 20/400. Families and friends are more likely to be aware of blindness compared to visual impairment. With that said, the overall incidence of blindness was estimated to be 0.04 percent of the population. Therefore, the chance that someone has a personal relationship and awareness of someone suffering from vision loss related to myopia is overall fairly small.
Myopia-related pathology occurs predominantly in the older population. As we know, progressive myopia is more of a concern in childhood. When discussing the pathologic risks we are forecasting well into the future. Parents may not be motivated when discussing complications that may occur 20 plus years down the road. Considering that the incidence of visual impairment is more common in the older population, how many of their family and friends are aware of their visual challenges? As mentioned in point number two, a history of blindness is more likely to be shared with family members. A common response that I receive in the exam room when there is an affirmative response to a family history of eye disease, including glaucoma and macular degeneration, is, “yes, but they were old.” I believe we need to continue to educate our patients that our goals for a lifetime of healthy eyes and normal vision is expected through the geriatric years.
This begs the question: What can we do to improve the general population’s understanding of the pathology associated with myopia? I believe it starts with eye care practitioners taking a more active approach in curbing the progression of myopia. According to a poll by Contact Lens Spectrum,3 42 percent of respondents reported actively practicing myopia control, which is a great sign for the future of the myopia field. This number is expected to grow with the recent U.S. FDA approval of CooperVision’s MiSight contact lens, the first product approved with the indication of slowing the progression of myopia. This may open the door for other contact lenses that similarly create peripheral myopic defocus, such as orthokeratology or NaturalVue 1 day multifocals.
Additionally, publications such as Review of Myopia Management and meetings such as the Global Myopia Symposium will only aid in the awareness of myopia management in the field. If practitioners, researchers, and industry continue beating the drum regarding pathology associated with myopia, it is only a matter of time before that information is absorbed by the general population, which will help free up our most valuable resource, time.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-660. doi:10.1016/j.preteyeres.2012.06.004
- Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018;102(7):855-862. doi:10.1136/bjophthalmol-2017-311266
- Contact Lens Spectrum, Volume: 35, Issue: January 2020, page(s): 18, 19, 21-25

Daniel Press, OD, FCOVD, is Clinical Director of Park Ridge Vision in Park Ridge, IL. Email him at drpress@prvisioncare.com. This article is sponsored by Visioneering Technologies, Inc. (VTI) MLT-GBL-NVM-WE2











