March 14, 2019
By Julie Tyler, OD, and Heidi Wagner, OD, MPH
Review of Optometry, January 2019
We are at a tipping point whereby treatments to curtail the progression of myopia are moving beyond the research and specialty clinic setting into the primary eye care practice environment. It is clear that myopia is on the rise—likely for a variety of reasons including, but not limited to, an increase in near-work demands and decrease in time outdoors.1,2 By 2050, nearly five billion people worldwide will have myopia compared with two billion in 2010.3While it is also clear that genetics play a role in the risk for developing myopia, inheritance patterns alone do not seem to account for the significantly increasing rate of myopic refractive error.4,5
Furthermore, the rise in myopia has public health significance: In addition to the daily increased reliance on spectacles and other vision correction by people with myopia, there is also an inherent risk of ocular comorbidities associated with this type of refractive error that may permanently and negatively affect vision, including increased risk of peripheral retinal degeneration, retinal detachments, myopic maculopathy, choroidal neovascular membrane and glaucoma.6
This discussion of pharmaceutical interventions, prescription modifications, orthokeratology (ortho-K) and soft bifocal/multifocal contact lens prescriptions is focused on the management of children and young adults. With regards to myopia interventions, recent research presents the most compelling evidence for ortho-K, bifocal/multifocal soft contact lenses and low-dose atropine.7–9 It should be noted that these interventions are not approved by the United States Food and Drug Administration (FDA); therefore, these options are off-label applications in the United States. Optometrists should present to parents such information as part of the informed consent process.
Ortho-K lenses allow patients to enjoy correction-free vision until they reapply them at bedtime, as corneal reshaping occurs overnight.
Atropine
The exact mechanism of action for slowing the progression of myopia with atropine is not well understood; notably, researchers have observed that low-dose atropine significantly reduces the progression of refractive error but has a lesser effect on axial length.10
Atropine is an anticholinergic agent (muscarinic antagonist) that competitively binds to receptors with acetylcholine or other agonists. In the eye, atropine is known to induce mydriasis by blocking contraction of the circular pupillary sphincter muscle—allowing the radial iris dilator muscle to contract and cause paralysis of accommodation (cycloplegia). For years, atropine and other mydriatic-cycloplegic agents have been used as part of the comprehensive management of anterior uveitis, but more recent studies have considered and compared treatments with atropine at levels ranging from 0.01%, 0.1% and 1.0% for myopia progression/control.11,12
Initially, 1% atropine was proposed as a method to delay or deter development of myopia.13 Unfortunately, side effects, such as burning or stinging of the eyes, conjunctival injection, blurred vision and systemic symptoms including flushing, tachycardia and restlessness, irritability or anxiety proved to be clinically significant enough to limit customary treatment. Additionally, higher concentrations of atropine were associated with a greater rebound effect when the medication was discontinued.10,14,15 Fortunately, continuing research has shown that lowering the concentration of atropine continues to result in measurable slowing of myopia progression while also allowing for tolerable side effects and a sustained effect in modulating the refractive error. 10,11,14,15 Thus, low-dose (0.01%) atropine can help slow myopia progression while minimizing the rebound effect and without noticeably increasing pupil size or blurring near vision.
Additional study is needed to understand how to optimize treatment regimens for individual patients based upon age, refractive error and other patient characteristics.10 It remains to be seen whether this treatment option will be less protective for ocular pathology if it exerts less effect on axial length.
While using atropine to manage myopia progression, patients also require correction for their current level of ametropia; therefore, spectacles are still necessary for many children on atropine therapy who already have developed myopia. For some children and parents who would prefer only one “method” of managing their refractive status, optical corrections/contact lens management may be a preferable myopia control option. However, other children (and their parents) may not embrace the concept of wearing contact lenses and the associated lens care and adverse events such as infectious keratitis. In that subpopulation, spectacle wear and atropine would be the most effective treatment option.
Low-dose atropine requires compounding at a pharmacy, making availability and cost a potential deterrent. Patients or parents who choose this option should instill one drop in each eye at bedtime for optimal myopia control and minimal side effects. While most young patients do not report blurred near vision or photophobia with lower concentrations of atropine, practitioners may wish to prescribe progressive addition lenses and photochromic lenses for the occasional symptomatic patient. For example, in a previous study with 0.05%, 0.025% and 0.01% atropine eye drops, the accommodation amplitude was reduced by 1.98±2.82D, 1.61±2.61 D, and 0.26±3.04D, respectively.12
Further research may provide additional understanding regarding patients who may benefit from additional spectacles support.
Spectacles
Historically, many proposed that the effect of “myopic defocus” in some patients may contribute to the development or progression of myopia. If a child’s spectacles were undercorrected (one study proposed blur at +0.75DS), the patient might have a delay in myopic changes in the eye, including axial length measurements and refractive status.16 However, multiple studies evaluating undercorrection in children have suggested that under-prescribing either enhances or has no effect on myopia progression.16,17
Additional considerations for spectacle prescribing include the use of bifocal and single vision lenses to slow myopic progression. One study demonstrated some benefit of executive bifocals in children—especially in combination with prism—for mild myopia control with results comparable with the ortho-K and multifocal soft contact lens studies, in terms of axial length and refractive myopia control.18 The benefit was more effective in patients with low lags of accommodation. The results with executive bifocals differed from the COMET study, which used progressive lenses and also demonstrated minimal clinical applications.19 These results not only help support the theory of peripheral defocus as a contributor to myopic progression but also identify that some subsets of children may have clinically relevant benefits with spectacles to deter myopic progression.
While often not the primary myopia management strategy, the necessity of spectacles as an adjunct to therapy is still evident. Children who wear contact lenses should always have a back-up pair of glasses available in the case of an infection, ocular surface irritation and visual correction when not wearing contact lenses. Moreover, when binocular issues occur concurrently with myopia, spectacles—including the use of prism or bifocal lens types—may be key to achieving overall normal, single, clear binocular vision for patients prescribed low-dose atropine or contact lenses as their primary myopia management protocol.
Contact Lens Wear
In addition to slowing the progression of myopia, contact lens wear provides other benefits to children and adolescents who don’t enjoy wearing spectacles. It provides a necessary vision correction and has been shown to improve vision-specific quality of life in myopic children younger than 12 years of age.20 Research also shows that contact lens wear boosts self-esteem with regards to physical appearance, athletic competence and social acceptance.21 Soft multifocals and ortho-K contact lenses provide comparable efficacy (approaching 50%) with regards to slowing the progression of myopia.22 Given that the mechanism for myopia control with atropine appears to be different than the mechanism with contact lenses, combination methods may prove to be effective and are currently being investigated.23
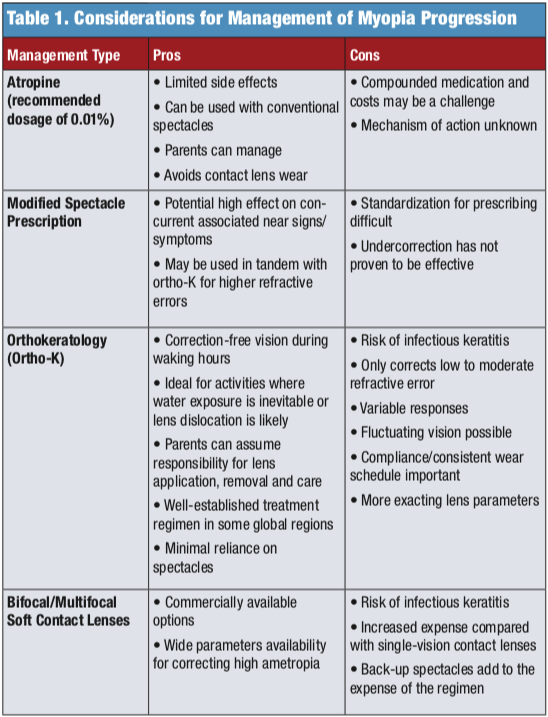
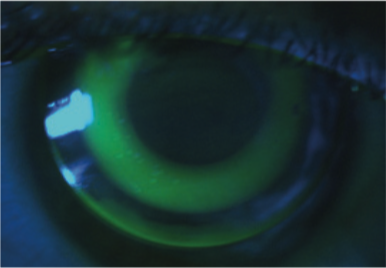
This myopia control method uses custom-designed gas permeable contact lenses that reshape the cornea to temporarily reduce refractive error. Paragon’s corneal reshaping treatment received FDA approval in 2002, while Bausch + Lomb’s Vision Shaping Treatment was approved in 2004. Notably, these approvals were for lenses prescribed for the correction of refractive error rather than for devices intended to reduce the progression of myopia.
While the exact lens parameters are proprietary, common characteristics of commercially available lens designs include a large diameter, small optic zone and a secondary (reverse) curve that is steeper than the base curve radius. This design enhances lens centration and promotes central epithelial cell compression. Fluid moves from area of central compression to surrounding areas of relief. The resultant mid-peripheral corneal thickening and shift of peripheral retinal defocus has been proposed as the primary myopia-inhibiting stimulus, although a cause-and-effect relationship has yet to be established.
Ortho-K is primarily used as a correction for low-to-moderate myopia (up to -6.00D) with or without astigmatism (up to -1.75D). Alternatively, the practitioner may elect to partially correct higher refractive errors with ortho-K lenses and prescribe spectacle over-correction for daytime use.24 At the other end of the refractive spectrum, low (less than or equal to 1.25D) refractive error is relatively easy to correct but the amount of peripheral defocus generated will be modest and possibly less effective in reducing myopic progression.
Initial lens selection may be based on empirical methods (spectacle prescription, keratometry, horizontal visible iris diameter), diagnostic lens fitting and/or corneal topographic analysis. Corneal topography allows for a more nuanced approach to identifying optimal candidates and is essential for monitoring lens position in overnight wear and performance over time. Such measures allow practitioners to assess corneal eccentricity and evaluate whether a toric peripheral curve system is indicated to optimize the lens-to-cornea fitting relationship. Toric lens designs are based on the sagittal height difference between corneal meridians rather than the manifest astigmatic refractive error. With-the-rule corneas are generally more amenable to treatment, as are steeper corneas.
Other prefit considerations include the patient’s and parents’ interest and motivation in wearing lenses. By design, ortho-K lenses entail applying lenses before bedtime. While the patient may initially exhibit apprehension in wearing rigid lenses, closed-eye wear minimizes lens awareness. Corneal reshaping occurs overnight so that patients enjoy correction-free vision until they reapply the lenses. Remaining lens-free during the day may be especially desirable for patients participating in sports such as swimming, where water exposure is inevitable, or other activities where lens dislocation is likely.
While more severe anterior segment disease is a contraindication to ortho-K lens wear, patients with mild dry eye or allergic symptoms may prefer overnight ortho-K to daily contact lens wear. The benefits of ortho-K must be considered against the risks (Table 1). Finally, ortho-K is a well-accepted treatment in some regions while relatively unknown in others; consequently, treatment decisions may also be influenced by the patient’s family and peers.
Uncorrected visual acuity may fluctuate during the fitting process or if the lenses are not worn on a consistent schedule. This may be of greater concern for older adolescents or young adults who are driving. Similarly, college-aged students may have erratic schedules and sleep patterns that result in an inconsistent wear schedule and variable vision.
Finally, the more exact fitting process may be appealing to some practitioners while off-putting for others. At minimum, the initial fitting process involves a baseline examination and fitting, dispensing visit, morning-after visit and follow-up visits until the desired endpoint is reached.
Periodic follow-up care is similar to that of other contact lens wearing subjects, with the caveat that more frequent visits may be merited, based upon on the overnight wear schedule and the needs of the individual patient.

Limiting time spent on electronic devices and length of near-distance work may reduce the chances of developing myopia.
In a previous retrospective study in the United States, the risk of microbial keratitis in ortho-K was similar to that of overnight wear of soft contact lenses.25 Corneal staining and lens binding have also been reported with this modality. Thus, successful ortho-K lens wear relies upon precise lens fitting, proper wear and care practices, periodic follow-up care and timely treatment of adverse events.
Multifocal Prescribing
The use of both multifocal spectacles and multifocal contact lenses for the management of myopia is something that many optometrists may be more comfortable with for the medical management of contact lens corneal reshaping therapy. In part, this is because most doctors write prescriptions for refractive error regularly. Compared with ordering compounded medications and the exam time and nuance of ortho-K, spectacle lenses are relatively easy to be made and multifocal contact lenses are available “off the shelf” (Table 2).
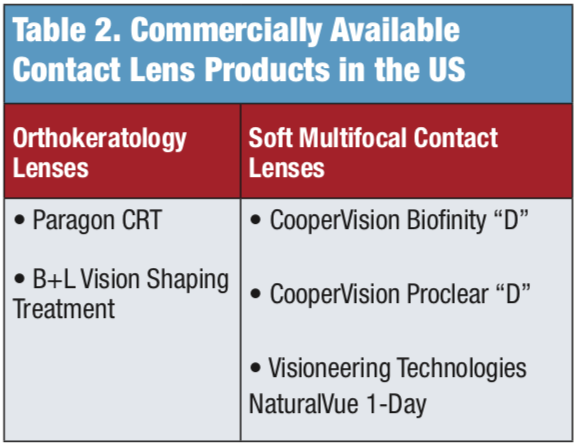
Soft multifocals. Center-distance daily wear contact lenses provide an alternative contact lens management option for reducing the progression of myopia.26-31 The central portion of the lens provides the distance myopic vision correction while the peripheral surround reduces hyperopic defocus. This, in turn, minimizes the stimulus for myopia progression by focusing the light in front of the peripheral retina. Commercially available lenses in the United States include CooperVision’s Biofinity and Proclear “D” monthly replacement lenses and Visioneering Technologies’ NaturalVue Multifocal 1-Day. Other products such as CooperVision’s dual-focus MiSight lens are available in Canada.
Soft multifocals are an excellent option for patients averse to overnight wear, those with refractive error beyond commercially available ortho-K parameters, or ortho-K dropouts. These lenses are also feasible for patients who wear contact lenses part-time, although reduced wearing time likely limits the lenses’ dampening effect on myopia progression. A previous study reported that the myopia modulating effect increased with daily wearing time, but the benefit plateaued after eight hours.30 The fitting process is relatively straightforward and comparable to other soft lens modalities with regards to chair time and follow-up schedule. Therefore, patients, parents and, in some cases, practitioners, may be more familiar with soft lenses and more readily embrace this treatment regimen. The Biofinity multifocal is available in spherical powers up to 8D and four add powers (+1.00D, +1.50D, +2.00D, +2.50D).
Proclear lenses provide even wider parameters. In clinical practice, the higher add power is initially selected to enhance the peripheral defocus, but the minus distance power may need to be increased slightly (typically -0.50D to -0.75D) to enhance distance vision. Occasionally, the add power may need to be reduced to optimize distance visual acuity.
The NaturalVue 1-day multifocal contact lenses, with an extended depth-of-focus center distance design, are manufactured with one add power up to +3.00D. They are currently available in spherical power up to -12.25D. Troubleshooting typically involves adding minus lens power to enhance distance vision.
In contrast, CooperVision’s MiSight is a daily disposable lens with two zones for vision correction and two for treatment (2D myopic defocus). It is not yet available in the United States but is available in Canada.31 The risks of adverse events are comparable to other soft lenses worn for daily wear.32
Beyond the specific therapies discussed previously, there are additional recommendations that we can make for our young patients when specific “additional” myopia management is not pursued. Notably, children who spend more time outdoors are less likely to develop myopia.33 While there is an emerging consensus that environment plays a factor, it is not well understood. Future recommendations for children might include participating in activities that encourage outdoor play for a period of time daily (“prescribed play”) as well as limiting time spent on electronic devices such as smartphones and tablets. It is also important to increase the working distance when using these devices.
Myopia, now commonly described as an epidemic, is a public health concern and common cause of visual impairment. Therefore, interventions designed to slow the onset of myopia and curtail its progression are of critical concern. Eye care professionals can potentially play an active role in modifying myopic outcomes. The needs and lifestyle of the individual patient should be taken into consideration when developing a treatment plan. By embracing strategies to reduce myopia progression, optometrists have the opportunity to reduce the economic burden of vision loss due to the condition.
Dr. Tyler is an associate professor and module chief of primary care for The Eye Care Institute at Nova Southeastern University in Davie, FL. Dr. Wagner is a professor of clinical optometry and director of extern programs at Ohio State University.
- Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet 2012;379(9827):1739-48.
- Jones-Jordan LA, Sinnott LT, Cotter SA, et al. Time outdoors, visual activity and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci. 2012;53(11):7169-75.
- Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42.
- Morgan IG, Rose KA. Myopia: is the nature-nurture debate finally over? Clin Exp Optom. 2018;102(1):3-17.
- Verhoeven VJ, Hysi PG, Wojciechowski R, et al. Genome-wide meta-analyses of multi-ancestry cohorts identify multiple new susceptibility loci for refractive error and myopia. Nature Genetics 2013;45(3):314-8.
- Ohno-Matsui K, Lai TY, Lai CC, et al. Updates of pathologic myopia. Prog Retin Eye Res. 2016;52:156-87.
- Si JK, Tang K, Bi HS, et al. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci. 2015;92(3):252-7.
- Li SM, Kang MT, Wu SS, et al. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow myopia progression in school-aged children: a meta-analysis. Ophthalmic Physiol Optic 2017;37(1):51-9.
- Gong Q, Janowski M, Luo M, et al. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol 2017;135(6):624-30.
- Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology. 2016; 123(2):391-9.
- Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia and efficacy at 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2). Ophthalmology. 2012;119(2):347-54.
- Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126(1):113-124.
- Dyer JA. Role of cycloplegics in progressive myopia. Ophthalmology. 1979;86(5): 692-4.
- Chia A, Chua WH, Wen L, et al. Atropine for the treatment of childhood myopia: changes after stopping atropine 0.01%, 0.1% and 0.5%. Am J Ophthalmol 2014;157:451-47.
- Tong L, Huang XL, Koh AL, et al. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine. Ophthalmology. 2009;116(3):572-9.
- Chung K, Mohidin N, O’Leary D. Undercorrection of myopia enhances rather than inhibits myopia progression. J Vision Research. 2002;42(22):2555-9.
- Li SY, Li Shi-Ming, Zhou YH, et al. Effect of undercorrection on myopia progression in 12-year-old children. Graefes Arch Clin Exp Ophthalmol 2015;253:1363-8.
- Cheng D, Woo G, Drobe B. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: Three-year results of a randomized clinical trial. JAMA Ophthalmol. 2014;132(3):258-64.
- Gwiazda J, Hyman L, Hussein M et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44(4):1492-500.
- Rah MJ, Walline JJ, Jones-Jordan LA, et al. Vision specific quality of life of pediatric contact lens wearers. Optom Vis Sci. 2010;87(8):560-6.
- Walline JJ, Jones LA, Sinnott L, et al. Randomized trial of the effect of contact lens wear on self-perception in children. Optom Vis Sci. 2009; 86(3):222-32.
- Walline JJ. Myopia control: a review. Eye Contact Lens 2016;42(1):3-8.
- ClinicalTrials.gov. Combined atropine with orthokeratology in childhood myopia control (AOK)-a randomized controlled trial. Available at: clinicaltrials.gov/ct2/show/NCT02955927. Accessed December 19,2018.
- Charm J, Cho P. High myopia—partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90(6):530-9.
- Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013;90(9):937-44.
- Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118(6):1152–1161.
- Sankaridurg P, Holden B, Smith E III, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52(13):9362–7.
- Walline JJ, Greiner KL, McVey ME, et al. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90(11):1207–14.
- Lam CS, Tang WC, Tse DY, et al. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese school- children: a 2-year randomised clinical trial. Br J Ophthalmol. 2014;98(1): 40–5.
- Cooper J, O’Connor B, Watanabe R, et al. Case series analysis of myopic progression control with a unique extended depth of focus multifocal contact lens. Eye Contact Lens. 2018;44(5):e16-24.
- CooperVision releases four-year data on landmark MiSight® 1 Day Contact Lens Study; pioneering approach slows myopia progression in children [press release]. CooperVision Public Relations; September 18, 2018. coopervision.com/our-company/news-center/press-release/coopervision-releases-four-year-data-landmark-misight-1-day. Accessed December 7, 2018.
- Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115(10):1655-62.
- Jones LA, Sinnottt LT, Mutti DO, et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48(8):3524-32.













