July 1, 2024
By Matthew J. Martin, OD, FIAOMC
Effective myopia management requires biometry with axial length progression and topographical assessment of the cornea. Much like the OCT is essential to glaucoma care, so is the use of biometry and topography essential to myopia management.
On a Monday evening at 6:30 pm, at the end of a long day full of complicated cases, emergencies, and staffing issues, we had a new patient comprehensive exam on a 7-year-old child. Precocious, intelligent, and enthusiastic, this was the perfect easy patient at the end of a long day. This young, Caucasian male child had no problems with his vision, was 20/20 in each eye, and the binocular and visual system assessment was excellent, with no need for glasses at the time. Almost as an afterthought, I took a quick look at the axial length (AL) measurement, which my staff runs on all children under the age of 18.
The Case for Routine Biometry
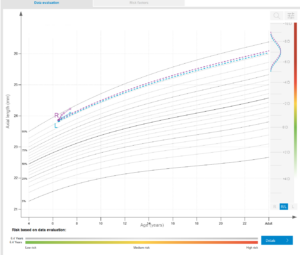
While the child did not have any appreciable glasses prescription, the axial length was 23.76 mm. That gave me cause for pause, and I asked the mom if she or her spouse wore glasses or contact lenses, but they both were emmetropes. I had my staff print up the myopia evaluation forms that our software creates so I could discuss myopia, nearsightedness, and the ramifications of this with the parent. Our software projected an adult AL of 25 mm to 26 mm and likely -7.00D to -7.50D of prescription. I spoke with the mother at length about this and sent her home with the paperwork. The front desk made an appointment for a follow-up AL measurement in four months. Unfortunately, the family did not show up for the follow-up and didn’t return our calls.
Monitoring Myopia Progression
Fast forward one year and two months later. The child is back in our schedule for a refraction and a second opinion. The family had decided to go to a different provider in our area for an exam, during which it was discovered the child was now a -2.00D myope. His AL measurement indicated a significant increase from 14 months earlier: 23.76 mm to 24.30 mm, a change of Δ0.54 mm. This was well beyond my “rule of thumb” rate of change of 0.2 mm or less per year.1,2
This new information led to a lengthy discussion with mom and dad about myopia, progression, and treatment options for slowing down this child’s very rapid progression. After reviewing myopia management options for this child, we decided on peripheral defocus contact lenses, and we began the process of establishing appointments for evaluation, fitting, and follow-ups, including AL measurements every four months.
This is a perfect example of how AL measurements and myopia management considerations could have saved us time and millimeters. Had the parents acted sooner by attending the follow-up appointment, could we have saved some of the myopia this child will bear as an adult? The answer is likely yes. Axial length is becoming the standard of care for pediatric eye care. After integrating AL measurements into all pediatric exams, I cannot imagine doing a child’s eye exam without this critical piece of information.
The Benefits of a Topographer
Another important piece of technology that demonstrates its value every day is our topographer. I purchased my first topographer for our office in 2002. To say it revolutionized my understanding of corneal physiology and corneal disease is an understatement. To fit orthokeratology, or any advanced contact lens, you need to know the shape, disposition, and eccentricity of the cornea. Topography allows a thorough understanding of these aspects of the front surface of the eye and informs all our decisions from soft lenses to scleral lenses. Implementing corneal topography into all our contact lens exams also allows us to build value into our contact lens evaluations.
During our myopia management evaluations, corneal topography plays an essential role. Many of our patients are interested in OrthoK, and it is often their number one choice for myopia management. It also happens to be my favorite myopia management modality due to how happy our patients are when we free them from glasses and contacts during the day.
Topography, and its close cousin tomography, are essential in diagnosing keratoconus as well. Placido disc topography maps the front surface of the cornea, while tomography uses Scheimpflug imaging to map both the front surface and posterior surface of the cornea. These two technologies have solved many of our office’s mystery patients, who had poor visual acuity that would not be corrected by other means. Having these instruments in the office has helped us to problem solve and diagnose many patients with underlying corneal disease, which would have gone undiagnosed in another office.
A Topography Success Story
An example of the essential nature of topography is a patient who elected to stop doing OrthoK after 15 years of wear. He had recently turned 25, finished college as an engineer, and wanted to pursue LASIK. He had started OrthoK when he was 10 years old at -3.00D. He stopped wearing his OrthoK retainers, and we managed the washout period using daily disposable contact lenses while he transitioned to baseline. After one week, he was essentially a -3.50D myope, and he held this power for about four weeks. However, upon examining the topographical difference maps, I noticed some minor changes that suggested we needed more time to return to baseline.
I prescribed 90 days of lenses and asked the patient to return to the clinic in 90 days. Upon returning, the patient’s prescription had stabilized at -3.75D. We made the referral to the surgeon, making sure all parties were aware of the history of OrthoK for 15 years. The surgeon waited another three months to be sure, and when nothing had changed, went forward with the procedure. Today, the patient is happy, stable, and loving life without the need for correction.
Effective myopia management requires biometry with axial length progression and topographical assessment of the cornea. Much like the OCT (Ocular Coherence Tomography) which was invented in 1991, and is essential to glaucoma care, so is the use of biometry and topography essential to myopia management.
Happy Fitting!
References
- Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, Klaver CCW. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018 May;96(3):301-309. doi: 10.1111/aos.13603. Epub 2017 Dec 19. PMID: 29265742; PMCID: PMC6002955.
- Sanz Diez P, Yang LH, Lu MX, Wahl S, Ohlendorf A. Growth curves of myopia-related parameters to clinically monitor the refractive development in Chinese schoolchildren. Graefes Arch Clin Exp Ophthalmol. 2019 May;257(5):1045-1053. doi: 10.1007/s00417-019-04290-6. Epub 2019 Mar 23. PMID: 30903312.