May 1, 2024
By Samrat Sarkar, PhD Candidate at the University of New South Wales
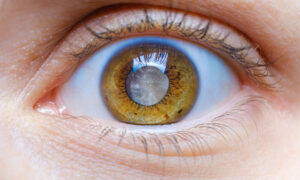
Myopia is a rapidly progressive ocular condition, and untreated myopia increases the global burden of blindness.1 Juvenile-onset myopia, also known as early-onset myopia or school myopia, commonly occurs between 8 and 13 years of age2 and mainly progresses through the teenage years.3 The prevalence of juvenile-onset myopia in school-going children is high in East Asia, ranging from 23.3% to 65.5%.4 Age of onset is considered one of the significant predictive factors for rapid myopia progression in myopic children.5 Optical, pharmacological, and combination therapies are available to slow myopia progression in children.6 However, none of the interventions can completely arrest myopia progression.7
It has been reported that several environmental risk factors, including near vision behavior and time outdoors moderate myopia development.8 Near vision behavior comprising viewing duration, viewing distance, and viewing breaks during near work has been linked with myopia development.9 Typically, near work can be categorized into reading, writing, drawing, and screen time (duration of exposure to computer, laptop, tablet, and smartphone screen).
With the rise of digital technology, children are now exposed to various devices from a young age. In fact, 95% of American teenagers own a smartphone,10 and 85% of the U.K. population aged 12 to 15 years uses smartphones daily.11 Closer viewing distances during any near visual tasks have been associated with myopia.9 It has been reported that children tend to hold smartphones or tablets at much shorter viewing distances compared to computer use and reading printed books.12 It is possible that prolonged exposure to smartphone or tablet screens with shorter viewing distances during childhood disrupts the accommodation and vergence demands, which may result in axial elongation.
Association Between Screen Time and Myopia
Several studies around the world have reported an association between screen time and prevalence of myopia,13-15 increased myopic spherical equivalent refraction,16 and axial length elongation.16,17 Some of these include:
- A longitudinal analysis with 1,496 Chinese school children before and during the COVID-19 pandemic reported greater than four hours per day of screen time as a risk factor for myopia.18
- The Myopia App study with a teenage Dutch population aged 12 to 16 years reported that four hours per day of smartphone use and continuous 20-minute use of smartphones were associated with more myopia.19
- Two studies with the North India population aged 5 to 15 years reported the risk of myopia development was eight times higher when children spent more than two hours per day playing video games compared to less than two hours per day studying in private schools.14 The study also found that the risk of myopia development was eight times higher when children spent more than four hours per week on computers and video games compared to no screentime.13
- A study with 6 to 7 year-old Irish children reported that more than two hours per day screen time was associated with myopic refraction.20
- A study with a 16 to 17-year-old Danish population revealed that after adjusting all confounding factors, screen time greater than six hours per day doubled the risk of myopia compared with screen time less than two hours per day.21
- Excessive screen time and less outdoor activity were reported in myopic children compared to non-myopic children in the 5 to 7 year-olds of a Spanish population.15
- A large-scale study with Chinese preschoolers with myopic parents aged between 2 and 7 years reported a strong association between exposure to electronic screens during 0 to 1 year of age and preschool myopia.22 However, the association between early screen exposure and myopia in school-going children has not yet been established.
A few studies also revealed no association between screen use and myopia in school-going children. For instance, a study with Chinese children aged between 6 and 14 reported no association between myopia and the duration of different digital device usage.16 However, axial length elongation was associated with increased smartphone and computer use, but not with tablet use and television watching.16 Another large-scale study with 34,644 Chinese school-going children with a median age of 11.9 years reported no association between myopia and screentime.23
Possible Reasons for Contradictory Findings
There are some possible reasons for the contradictory findings about the association between screen time and myopia in children. Firstly, most studies reported screen time based on parental-reported surveys, which may be biased and underestimate the child’s actual screentime.9 Secondly, a few studies have defined myopia based on self- or parental-reported questionnaires about the difficulty in seeing at a distance24,25 instead of standardized refraction measures after cycloplegia. Finally, studies have reported only the association between near work duration and myopia, not individual associations between mobile/ tablet/ computer screen time and myopia.26,27 Also, there is a lack of information about the timeframe and duration of initial exposure to the screen among myopic children and the age of onset of myopia.
Requirement of More Research on Screen Time and Myopia in the Future
In this era of digitalization, more scientific research on the impact of screen time on childhood myopia progression is required. Specifically, randomized clinical trials on childhood myopia progression with reducing screen time, reading printed books, and spending more time outdoors as an individual myopia control intervention and their interactions are required. Self-reported or parental-reported surveys are subject to bias9 and hinder the actual quantification of screen time. Therefore, studies on the association between objective or real-time quantification of screen time with digital (mobile or tablet or computer) apps,19 or with wearable sensors like Vivior that can track the duration of smartphone or laptop use and myopia, are recommended in the future.
References
- Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthalmol Vis Sci. 2020;61(4):49.
- Bullimore MA, Lee SS, Schmid KL, Rozema JJ, Leveziel N, Mallen EAH, et al. IMI-Onset and Progression of Myopia in Young Adults. Invest Ophthalmol Vis Sci. 2023;64(6):2.
- Zadnik K, Sinnott LT, Cotter SA, Jones-Jordan LA, Kleinstein RN, Manny RE, et al. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol. 2015;133(6):683-9.
- Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020;20(1):27.
- Chua SY, Sabanayagam C, Cheung YB, Chia A, Valenzuela RK, Tan D, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36(4):388-94.
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci. 2019;96(6):463-5.
- Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Prog Retin Eye Res. 2021;83:100923.
- Wildsoet CF, Chia A, Cho P, Guggenheim JA, Polling JR, Read S, et al. IMI – Interventions Myopia Institute: Interventions for Controlling Myopia Onset and Progression Report. Invest Ophthalmol Vis Sci. 2019;60(3):M106-m31.
- Gajjar S, Ostrin LA. A systematic review of near work and myopia: measurement, relationships, mechanisms and clinical corollaries. Acta Ophthalmol. 2021.
- Vogels E A G-WR, Massarat N. Teens, Social Media and Technology 2022 2022 [Available from: https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/.
- Ofcom. Children and Parents: Media Use and Attitude Report 2017 [Available from: https://www.ofcom.org.uk/__data/assets/pdf_file/0020/108182/children-parents-media-use-attitudes-2017.pdf.
- Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom. 2017;100(2):133-7.
- Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Menon V, et al. Prevalence of myopia and its risk factors in urban school children in Delhi: the North India Myopia Study (NIM Study). PLoS One. 2015;10(2):e0117349.
- Singh NK, James RM, Yadav A, Kumar R, Asthana S, Labani S. Prevalence of Myopia and Associated Risk Factors in Schoolchildren in North India. Optom Vis Sci. 2019;96(3):200-5.
- Alvarez-Peregrina C, Sánchez-Tena M, Martinez-Perez C, Villa-Collar C. The Relationship Between Screen and Outdoor Time With Rates of Myopia in Spanish Children. Front Public Health. 2020;8:560378.
- Liu S, Ye S, Xi W, Zhang X. Electronic devices and myopic refraction among children aged 6-14 years in urban areas of Tianjin, China. Ophthalmic Physiol Opt. 2019;39(4):282-93.
- Chua SY, Ikram MK, Tan CS, Lee YS, Ni Y, Shirong C, et al. Relative Contribution of Risk Factors for Early-Onset Myopia in Young Asian Children. Invest Ophthalmol Vis Sci. 2015;56(13):8101-7.
- Cui L, Zhou H, Lou X, Chen T, Guo Y, Li J, et al. Effects of behaviors and surrounding environment on myopia before and during the COVID-19 pandemic: a longitudinal analysis of children and adolescents in China. Z Gesundh Wiss. 2023:1-13.
- Enthoven CA, Polling JR, Verzijden T, Tideman JWL, Al-Jaffar N, Jansen PW, et al. Smartphone Use Associated with Refractive Error in Teenagers: The Myopia App Study. Ophthalmology. 2021;128(12):1681-8.
- Harrington S, O’Dwyer V. The association between time spent on screens and reading with myopia, premyopia and ocular biometric and anthropometric measures in 6- to 7-year-old schoolchildren in Ireland. Ophthalmic Physiol Opt. 2023;43(3):505-16.
- Hansen MH, Laigaard PP, Olsen EM, Skovgaard AM, Larsen M, Kessel L, et al. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 Eye Study. Acta Ophthalmol. 2020;98(3):315-21.
- Yang GY, Huang LH, Schmid KL, Li CG, Chen JY, He GH, et al. Associations Between Screen Exposure in Early Life and Myopia amongst Chinese Preschoolers. Int J Environ Res Public Health. 2020;17(3).
- Zhang D, Sun B, Wu M, Liu H, Zhou L, Guo L. Prevalence and associated factors of myopia among school students in Shenyang, China: a cross-sectional study. Front Public Health. 2023;11:1239158.
- Huang L, Kawasaki H, Liu Y, Wang Z. The prevalence of myopia and the factors associated with it among university students in Nanjing: A cross-sectional study. Medicine (Baltimore). 2019;98(10):e14777.
- Toh SH, Coenen P, Howie EK, Mukherjee S, Mackey DA, Straker LM. Mobile touch screen device use and associations with musculoskeletal symptoms and visual health in a nationally representative sample of Singaporean adolescents. Ergonomics. 2019;62(6):778-93.
- Hinterlong JE, Holton VL, Chiang CC, Tsai CY, Liou YM. Association of multimedia teaching with myopia: A national study of school children. J Adv Nurs. 2019;75(12):3643-53.
- Lin Z, Vasudevan B, Mao GY, Ciuffreda KJ, Jhanji V, Li XX, et al. The influence of near work on myopic refractive change in urban students in Beijing: a three-year follow-up report. Graefes Arch Clin Exp Ophthalmol. 2016;254(11):2247-55.