sponsored content
November 16, 2020
By Noel Brennan, BOptom, MScOptom, PhD, FAAO
 First things first… in referring to every myopic child, we are talking about primary myopia, otherwise known as school myopia or juvenile myopia. Myopia secondary to syndromic conditions is not known to be susceptible to myopia control treatments. (As a simple rule for assessing a possible syndrome, if the number of diopters exceeds the age of the child, refer for specialist work-up).
First things first… in referring to every myopic child, we are talking about primary myopia, otherwise known as school myopia or juvenile myopia. Myopia secondary to syndromic conditions is not known to be susceptible to myopia control treatments. (As a simple rule for assessing a possible syndrome, if the number of diopters exceeds the age of the child, refer for specialist work-up).
Second, by child, we mean children aged 12 and under.
So, why should we treat every myopic child under 12 years of age? Progression of myopia from childhood through to mature age has not been well documented. A black hole exists between the ages of 18 and 40 where there is a dearth of information on refractive progression. The minimum we do know is that age of onset is our best guide to likely development of higher amounts of myopia later in life.1,2
New Data From Finland Measures Refractive Trajectory
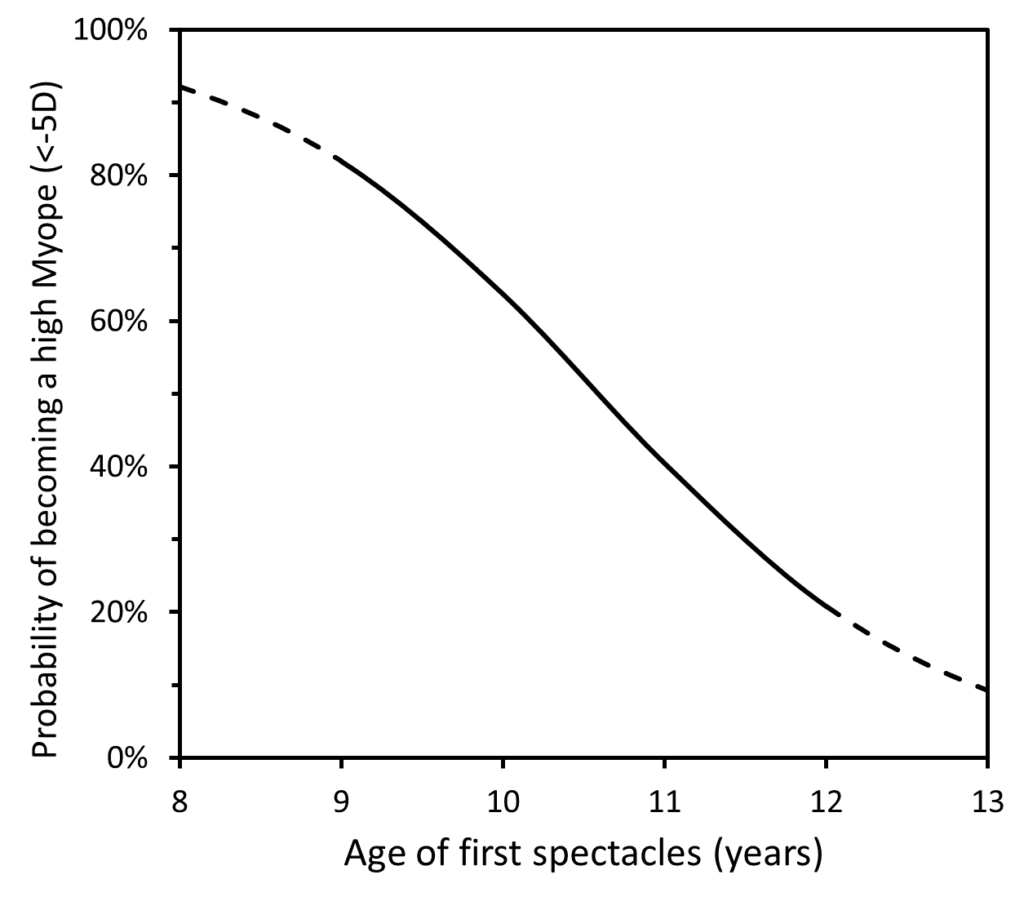
A recent paper from Finland looked at refractive trajectory of a population for whom data were available for first myopic spectacle prescription (aged 8 to 12) through to adulthood at age of early- to mid-30s, a follow-up of 22 years.3 While there are some methodological challenges in the paper, the results are nonetheless illuminating, revealing a high risk of becoming highly myopic in this age group. The figure below shows the modelled chance of becoming highly myopic (< -5D) at a given age. Over 80 percent of those getting their first myopic spectacles at age 9 become highly myopic, and over 20 percent of 12-year-olds are also prone to becoming highly myopic. Hu et al. reported somewhat lower risk but did not follow-up for as long (12 years) and used -6D as the threshold for high myopia.2 However, it is notable that they found over 25 percent of 11-year-olds diagnosed with myopia had axial lengths of over 26 mm by 23 years of age.
Why is this important? Bilateral blindness or low vision will develop “in more than one in three persons with high myopia”.4 But, furthermore, it is wrong to regard “high” myopia as the ultimate differentiation point for risk of disease. In one study, participants with low (-3.0 D < SE ≤ -0.5 D), moderate (-5.0 D < SE ≤ -3.00D), and high myopia (SE ≤ -5.00D), showed prevalence of myopic macular degeneration (MMD) among those aged over 70 years of 31.1 percent, 47.7 percent, and 65.0 percent, respectively.5 Yes – you read that correctly – low myopes were found to have greater than 30 percent chance of ultimately developing MMD. In that study, over 50 percent of all patients with MMD were not high myopes.
As a community, we are clearly not yet sensitized to the complications associated with myopia and their grave implications. Since the children of the myopia epidemic were largely born after 1970, this population has not yet reached the age of 50 when the associated complications begin to escalate. But, in coming decades, we will see myopia take shape as the biggest eye health threat. For example, Fricke et al. predict a 13-fold increase in the number of people with vision impairment due to MMD from the year 2000 to 2050.6 The outlook in the most endemic regions of Asia is particularly dire, with 1 in 10 people predicted to develop visual impairment.7 But the West is not immune to the problem.
Can You Follow For A Year Before Beginning Myopia Management?
You may ask, “Why can’t I follow the child for a year and see if they are a fast progressor?” Unfortunately, the error in measurement of refractive error progression is about the same as the progression rate we are trying to measure.8 Our ability to isolate those myopic children who will not become highly myopic later in life is poor. And suppose you did identify that a child has progressed by, let’s say, a diopter or a diopter and a half over a year – that’s progression you now can’t take back. And every diopter reduction in progression lessens the risk of MMD by about 40 percent.9 The risks associated with, say, increasing outdoor time and use of daily disposable myopia control contact lenses are minimal compared to those associated with myopia associated complications later in life.10
As for teenagers, there is room for some discretion in the case of low levels of myopia. But we should be cognizant of the fact that the Finnish study mentioned above showed further progression of more than two diopters on average from age 13.9 years to early to mid-thirties.3
Regardless of the age treatment was initiated, once myopia control therapy has begun, myopia stabilization cannot be differentiated from an effective myopia control therapy. This evidence of adult progression supports that, if well-accepted, myopia control therapy may be continued beyond the teenage years.
Eye care is likely to move in the direction of treating all young, myopic children as the standard of practice in the near future. Not treating a myopic child should be the exception to the rule. Get ahead of the curve and proactively recommend treatment for all myopic children 12 years of age and under.
Figure: Probability of becoming a high myope (< -5D) by age of first spectacles, modelled using data from Table 2 of Pärssinen and Kauppinen.3

Noel A. Brennan, MScOptom, PhD, FAAO, is Clinical Research Fellow at Johnson & Johnson Vision Care, where he has been for the past nine years. Prior to that he co-directed a privately owned research consulting company and, before that, was a professor at the University of Melbourne. Under a Senior Fulbright Scholarship, Dr. Brennan was also visiting scholar in the Department of Surgery at Stanford University. He was recently named one of the 30 most influential people in the contact lens field over the past 30 years in Contact Lens Spectrum.
References
- Chua SY, Sabanayagam C, Cheung YB, et al. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Ophthal Physiol Opt 2016;36:388-94.
- Hu Y, Ding X, Guo X, et al. Association of Age at Myopia Onset with Risk of High Myopia in Adulthood in a 12-Year Follow-up of a Chinese Cohort. JAMA Ophthalmol 2020.
- Pärssinen O, Kauppinen M. Risk Factors for High Myopia: A 22-Year Follow-up Study from Childhood to Adulthood. Acta Ophthalmol 2019;97:510-8.
- Verhoeven VJ, Wong KT, Buitendijk GH, et al. Visual Consequences of Refractive Errors in the General Population. Ophthalmology 2015;122:101-9.
- Wong YL, Sabanayagam C, Ding Y, et al. Prevalence, Risk Factors, and Impact of Myopic Macular Degeneration on Visual Impairment and Functioning among Adults in Singapore. Invest Ophthalmol Vis Sci 2018;59:4603-13.
- Fricke TR, Jong M, Naidoo KS, et al. Global Prevalence of Visual Impairment Associated with Myopic Macular Degeneration and Temporal Trends from 2000 through 2050: Systematic Review, Meta-Analysis and Modelling. Br J Ophthalmol 2018.
- Tideman JW, Snabel MC, Tedja MS, et al. Association of Axial Length with Risk of Uncorrectable Visual Impairment for Europeans with Myopia. JAMA Ophthalmol 2016;134:1355-63.
- Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in Myopia Control. Prog Retin Eye Res (in press) 2020.
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5.
- Gifford KL. Childhood and Lifetime Risk Comparison of Myopia Control with Contact Lenses. Contact Lens Ant Eye 2020;43:26-32.
This article is sponsored by Johnson & Johnson Vision.
PP2020OTH11910











