April 3, 2023
By Dwight Akerman, OD, MBA, FAAO, FBCLA, FIACLE
Myopia can no longer be considered a benign refractive condition with few, if any, long-term eye health consequences. Instead, myopia must be considered an axial length disease. The refractive changes associated with myopia are a manifestation of an increase in axial length so that the optical components of the eye are no longer aligned. Axial length is the combination of anterior chamber depth, lens thickness, and vitreous chamber depth, and it is the most significant contributor to refractive error.
Ocular morbidity increases per millimeter of axial length. These eye health complications include myopic macular degeneration, retinal detachment, primary open angle glaucoma, macular hole, retinoschisis, and nuclear and posterior subcapsular cataract. With the exception of cataracts, myopic complications have a substantial risk of permanent visual impairment. Reducing axial length growth is the most critical goal for treating childhood myopia.
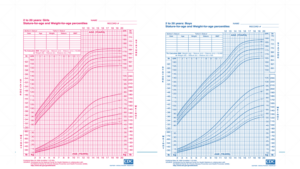
Axial length does not have a stable growth rate with age, nor is it similar among the sexes and ethnicities. Therefore, axial length should be related to growth curves per gender and ethnicity. Recent research has provided insights into typical axial length growth rates, enabling the risk of myopia to be assessed, with normative values published for cohorts of European and Asian children. The collected data were reported as percentiles, which is terminology parents are very familiar with. For example, most pediatricians present parents with stature-for-age and weight-for-age percentile charts at their child’s annual physical. The availability of percentile data on large population samples will help eye care professionals match patient age, refractive error, and axial length to a predicted outcome.
Axial length measurement has not traditionally been considered part of mainstream optometry and certainly not myopia management. The same could have been said for using an OCT 10-15 years ago. Just as optometrists have embraced OCTs for managing ocular disease, eye care professionals should aim to do the same for axial length measurement in myopia management.
There are two main options for measuring axial length: ultrasound biometry and optical biometry. A-scan ultrasound biometry is a more challenging technique to use on children due to the contact nature of the instrument and is less accurate than optical biometry. Therefore, optical biometry is the preferred technique to measure axial length in children. There are many options available for optical biometry, covering a range of budgets. Most instruments are easy to use on children and are non-invasive.
Once you have prescribed a myopia management strategy for a child or adolescent, it is necessary to monitor that patient to determine whether the chosen therapy is slowing myopia progression. Progression is not just the change in refractive error over time but also the change in axial length. Measuring and monitoring only one of the components could be considered to be doing only half the job. Axial length measurement with an optical biometer is considered the gold standard of myopia management, and investing in the equipment required to measure axial length is ultimately an investment in the long-term eye health of your pediatric myopes.
When parents are reluctant to enter the realm of myopia management, often stating that simple correction has been perfectly suitable for themselves, ECPs need to find a way to convince them that there is good evidence to be proactive and intervene early. Axial elongation, and subsequent increase in myopia, result in an increased risk of ocular complications associated with myopia. Being able to point to their child’s axial length measurement and show the likely trajectory and the associated risks provides compelling evidence that intervention is appropriate.
For additional information on the importance of managing progressive myopia with an optical biometer, I recommend reading a paper written by Professor Debbie Jones from the University of Waterloo and CORE, Measure Axial Length to Guide Myopia Management, and also How to Interpret Axial Length Measurements written by Dr. Thomas Naduvilath from BHVI.
Reducing axial length growth is the most critical goal when treating myopia. Axial length rather than myopic refractive error should be the primary target for myopia management. Assessing axial length at each visit with an optical biometer means practicing at the highest level and fulfilling one’s duty of care.
Best professional regards,
Dwight H. Akerman, OD, MBA, FAAO, FBCLA, FIACLE
Chief Medical Editor
dwight.akerman@gmail.com