October 1, 2021
By Xiao Nicole Liu, MOptom, PhD Candidate at the Brien Holden Vision Institute
Recognition of sleep as a component of the approximately 24-hour sleep/wake cycle mediated by circadian rhythm can lead to better interpretations of its relationship with myopia.

Sleep plays a vital role in children’s health. It can affect the wellbeing of a child in various aspects, from physical development to cognitive performance.1 Although the significance of sleep has long been acknowledged, incorporating sleep hygiene into ocular health promotion messages and strategies is relatively rare. Understanding the relationship between sleep and childhood myopia provides evidence to advocate for better sleep hygiene in children.
Sleep Duration and Myopia
Despite the fact that sleep is a multidimensional construct, to date, the majority of myopia studies that investigated the effect of sleep focused primarily on the duration of sleep. Shorter sleep duration was associated with an increased risk and severity of myopia in a number of studies. A study of 3,625 Korean teenagers (age range 12 to 19 years) reported that subjects who had more than nine hours of sleep were 41% less likely to be myopic compared to those who slept less than five hours per night.2 Similarly, a survey of 15,316 Chinese children (age range 6 to 18 years) indicated an increased risk for myopia among those who slept seven hours or less per night compared to those who slept more than nine hours per night.3 However, other studies found no relationship between sleep duration and myopia.4-8 Possible explanations for such discrepancies include limitations in sleep measurement vehicles, varied age of study samples, and differences in other environmental or behavioral factors.
Bedtime and Myopia
Nevertheless, there are other characteristics of sleep that are of equal, if not more, importance as sleep duration in terms of evaluating health outcomes.1, 9 For instance, sleep onset latency, daily variability, and timing of sleep are three characteristics that have recently been highlighted in myopia research. A longitudinal study observed significantly shorter latency and greater variability of sleep duration across days and seasons in myopes aged 10 to 15 years. With shorter latency being an indicator of sleep deprivation and greater variability of sleep often associated with “social jetlag,” findings of this study allude to a relationship between disturbances to children’s body clocks, their circadian rhythm, and myopia.8 Meanwhile, in another study, later bedtime was identified as a constant risk factor for higher prevalence, higher incidence (Figure 1), and greater progression of myopia in children.6 This significant association across incidence and progression also indicates the involvement of circadian rhythm in childhood myopia development.
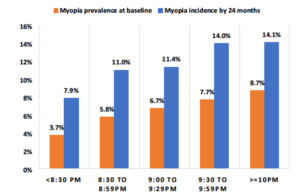
Figure 1. Trend of myopia baseline prevalence and 24-month incidence by bedtime categories (adapted from Liu et al.6)
Circadian Rhythm and Myopia
Recognition of sleep as a component of the approximately 24-hour sleep/wake cycle mediated by circadian rhythm can lead to better interpretations of its relationship with myopia. Animal studies demonstrated that regular light/dark or wake/sleep cycles are critical for normal ocular growth, and alterations to this cycle would result in refraction shifts.10-12 In human studies, genetic factors controlling circadian rhythms were identified to be involved in myopia development.13 This connection between sleep and myopia is further strengthened by understanding the contribution of the intrinsically photosensitive retinal ganglion cells (ipRGCs) in the human retina to circadian entrainment. A subset of ipRGC axons project to the suprachiasmatic nucleus (SCN), the primary pacemaker in the hypothalamus, to mediate the synchronization of the body clock to the solar day.14 Unlike rods and cones, which hyperpolarize in response to light, ipRGCs depolarize when perceiving light.15 This light-evoked depolarization of ipRGCs enables photic suppression of melatonin, a hormone that releases in dim light or darkness and engages in the physiological regulation of sleep.16 Therefore, exposure to bright light prior to bedtime, particularly to light with a peak wavelength close to the peak sensitivity of ipRGCs (~482nm), would trigger melatonin suppression and consequently cause disturbance to sleep.
Other Sleep Problems Observed in Myopes
In addition to the aforementioned sleep problems, studies have shown that compared with non-myopic subjects, myopes exhibited significantly higher serum melatonin concentration in the morning,17 delayed circadian timing and sleep onset in the evening, and preferences for an evening-type lifestyle.18
In summation, the body of evidence for a complex relationship between sleep or circadian disturbance and myopia is mounting, even though underlying mechanisms are yet to be elucidated. Encouraging sleep hygiene, such as early to bed and reducing bright light exposure before bedtime, in ocular health promotion messages and strategies targeting children should be essential and executed with urgency.
Xiao Nicole Liu, MOptom, is a PhD candidate at the Brien Holden Vision Institute, supervised by Prof. Padmaja Sankaridurg and A/Prof. John Thomas Naduvilath.
References
- Matricciani, L., et al., Children’s sleep, and health: A meta-review. Sleep Med Rev, 2019. 46: p. 136-150.
- Jee, D., I.G. Morgan, and E.c. Kim, Inverse relationship between sleep duration and myopia. Acta Ophthalmologica, 2016. 94(3): p. e204-e210.
- Gong, Y., et al., Parental myopia, near work, hours of sleep and myopia in Chinese children. Health, 2014. 2014.
- Zhou, Z., et al., Disordered sleep and myopia risk among Chinese children. PLoS One, 2015. 10(3): p. e0121796.
- Sensaki, S., et al., Sleep duration in infants was not associated with myopia at 3 years. Asia-Pacific Journal of Ophthalmology, 2018. 7(2): p. 102-108.
- Liu, X.N., et al., Sleeping late is a risk factor for myopia development amongst school-aged children in China. Sci Rep, 2020. 10(1): p. 17194.
- Wei, S.-F., et al., Sleep Duration, Bedtime, and Myopia Progression in a 4-Year Follow-up of Chinese Children: The Anyang Childhood Eye Study. Investigative Ophthalmology & Visual Science, 2020. 61(3): p. 37-37.
- Ostrin, L.A., et al., Sleep in Myopic and Non-Myopic Children. Transl Vis Sci Technol, 2020. 9(9): p. 22.
- Bin, Y.S., Is Sleep Quality More Important Than Sleep Duration for Public Health? Sleep, 2016. 39(9): p. 1629-1630.
- Lauber, J.K. and J. Shutze Jv Mcginnis, Effects of exposure to continuous light on the eye of the growing chick. Proc Soc Exp Biol Med, 1961. 106: p. 871-2.
- Stone, R.A., et al., Photoperiod, early post-natal eye growth, and visual deprivation. Vision Res, 1995. 35(9): p. 1195-202.
- Nickla, D.L. and K. Totonelly, Brief light exposure at night disrupts the circadian rhythms in eye growth and choroidal thickness in chicks. Exp Eye Res, 2016. 146: p. 189-195.
- Hysi, P.G., et al., Meta-analysis of 542,934 subjects of European ancestry identifies new genes and mechanisms predisposing to refractive error and myopia. Nat Genet, 2020. 52(4): p. 401-407.
- Gooley, J.J., et al., A broad role for melanopsin in nonvisual photoreception. J Neurosci, 2003. 23(18): p. 7093-106.
- Hankins, M.W., S.N. Peirson, and R.G. Foster, Melanopsin: an exciting photopigment. Trends Neurosci, 2008. 31(1): p. 27-36.
- Berson, D.M., Strange vision: ganglion cells as circadian photoreceptors. Trends Neurosci, 2003. 26(6): p. 314-20.
- Kearney, S., et al., Myopes have significantly higher serum melatonin concentrations than non-myopes. Ophthalmic Physiol Opt, 2017. 37(5): p. 557-567.
- Chakraborty, R., et al., Myopia, or near-sightedness, is associated with delayed melatonin circadian timing and lower melatonin output in young adult humans. Sleep, 2021. 44(3).














