sponsored content
November 1, 2021
By Azinda Morrow, OD, FAAO
Although OrthoK fitting can appear complex, breaking down the practice protocol into straightforward steps can simplify the process.

Orthokeratology is an ever-expanding field of clinical myopia management. Careful consideration is necessary for identifying proper patient candidates for OrthoK treatment, and fitting involves a thorough understanding of specialty lenses. Even with early visual success, appropriate follow-up schedules and protocols are required to ensure optimal ocular health and myopia management for these patients.
What Makes an Ideal OrthoK Candidate?
Not all patients are proper candidates for OrthoK. First, from a “data-only” perspective, it is paramount to get an accurate baseline refraction (preferably cycloplegic refraction) and topographical measurements. Flat keratometry values should be between 40.00 and 46.00, with limited corneal astigmatism. Most topographers will also provide important values such as elevation differences and horizontal visible iris diameter (HVID), which help choose a spherical versus toric lens design, and overall diameter. In addition, as refractive error is being purposefully altered, pre- and post-treatment axial length measurements are critical in monitoring the patients’ underlying myopia.
Personality, hobbies, and degree of child versus parent involvement can aid in proper patient selection. Because all OrthoK lens wear and care are done at home, with appropriate education, parents can be more involved with lens handling and care, allowing the child to have fewer responsibilities. Patients who wear OrthoK lenses are less prone to potential ocular health risks during the day, which can reassure many patients and their families.
Once accurate baseline data is acquired, there are two options to initiate the fit — either empirically or with an in-office trial set. By providing refractive error, topographical, and HVID measurements to the manufacturer, an empirical lens order typically allows for a positive initial experience for patients with high “first lens success.” Conversely, with in-office fitting, lens fit troubleshooting can be performed before the initial lens order.
Tips Prior to Initial Lens Dispensing:
- Verify that vision should be clear and comfortable in each eye independently while wearing the lenses.
- The over-refraction of the lens should be a low hyperopic prescription (+0.50 to +1.00).
- Check that the lens fits appropriately.
- Ensure that patient, parent, or both have sufficient understanding of correct lens handling and care.
After dispensing the initial lenses, my protocol is to have the patient return for an immediate one-day follow-up (ideally in the morning), one to two weeks later, and one month after treatment initiation.
Follow-up Procedures
At the initial one-day follow-up, corneal health is of utmost importance. Typically, corneal health is adequate on the first follow-up, and an improvement in uncorrected visual acuity, reduction in residual refractive error, and topography indicating overnight lens wear is observed.
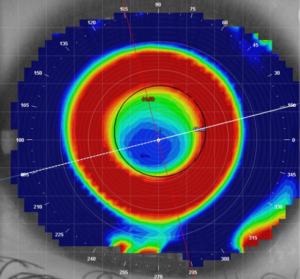
An example of a post-orthokeratology topography map with a well-centered, round treatment zone and robust paracentral steepening.
As further follow-ups occur, uncorrected vision should continue to improve to 20/20 in either eye within the first one to two weeks, with a reduction in myopic refractive error.
In addition, the treatment area and surrounding ring of steepening should become more prominent and defined. When any of these critical measurements (uncorrected visual acuity, residual refractive error, corneal health, and/or topography) are less than ideal, re-inserting the OrthoK lens in-office can assist in determining what aspects of the lens fit require changing to enhance the patient’s visual experience and ocular health.
How Do We Go About Troubleshooting?
Troubleshooting an OrthoK lens can seem daunting, but it is very straightforward. Begin by noting whether changes need to be made for visual, health, or comfort purposes. For example, visual issues, such as reduced uncorrected visual acuity, unexpected or quick regression of vision during the day, or subjective disturbances such as halos and glare, can indicate lens fit changes, i.e., a flatter base curve, tighter lens peripheries, or reduced lens sagittal depth. Performing serial topography maps at each visit is critical in determining lens centration and treatment effect. If corneal complications are present, it is vital to prioritize ocular health and determine if the patient requires lens fit adjustments, including higher oxygen-permeable materials, lubricants upon insertion of the lens, or improved lens-handling techniques.
It is essential to counsel your patients and families to set expectations of how often to monitor for myopia progression. Most often, it is recommended to re-evaluate myopia patients every six months, at minimum, although some clinicians choose to follow patients more frequently (every three to four months). Continue to use uncorrected visual acuity, residual refractive error, and corneal topographical maps for OrthoK patients. In addition, many multi-doctor practices use a written protocol to ensure all repeated measurements are performed consistently and accurately.
Although OrthoK fitting can appear complex, breaking down the practice protocol into straightforward steps can simplify the process. Best of all, the care provided to patients through this lens modality is truly rewarding. As the myopia epidemic worsens, a proper understanding of OrthoK candidacy, fitting, and monitoring will become critical for managing childhood myopia. By keeping apprised of new research and lens designs, eye care providers can make a lasting impact by offering personalized, creative care with OrthoK.
 Azinda Morrow, OD, FAAO, is an assistant clinical professor at the SUNY College of Optometry/University Eye Center and responsible for clinical supervision of students and residents in both the Cornea/Contact Lens and Myopia Management clinics. She earned her Doctor of Optometry degree from SUNY Optometry in 2017 and completed her residency in Cornea and Contact Lenses at the Illinois College of Optometry in 2018. Dr. Morrow teaches in the contact lens pre-clinical laboratories and engages in clinical research through the Clinical Vision Research Center, where she has been both a principal investigator and sub-investigator on multiple contact lens and myopia control studies. Dr. Morrow is also a fellow of the American Academy of Optometry, and a member of the American Optometric Association.
Azinda Morrow, OD, FAAO, is an assistant clinical professor at the SUNY College of Optometry/University Eye Center and responsible for clinical supervision of students and residents in both the Cornea/Contact Lens and Myopia Management clinics. She earned her Doctor of Optometry degree from SUNY Optometry in 2017 and completed her residency in Cornea and Contact Lenses at the Illinois College of Optometry in 2018. Dr. Morrow teaches in the contact lens pre-clinical laboratories and engages in clinical research through the Clinical Vision Research Center, where she has been both a principal investigator and sub-investigator on multiple contact lens and myopia control studies. Dr. Morrow is also a fellow of the American Academy of Optometry, and a member of the American Optometric Association.
This article is sponsored by Euclid.
References
- Cho, P, and Cheung, S. Retardation of Myopia in Orthokeratology (ROMIO) Study: A 2-Year Randomized Clinical Trial. Invest Ophthalmol Vis Sci. 2012 Oct 11;53(11):7077-85.
- Gifford, K., et al. IMI – Clinical Management Guidelines Report. Invest Ophthalmol Vis Sci. 2019 Feb 28;60(3): M184-M203.
- Hiraoka, et al. Long Term Effect of Overnight Orthokeratology on Axial Length Elongation in Childhood Myopia: A 5-Year Follow-up Study. Invest Ophthalmol Vis Sci. 2012 Jun 22;53(7):3913-9.
- Wildsoet, C., et al. IMI – Interventions for Controlling Myopia Onset and Progression Report. Invest Ophthalmol Vis Sci. 2019 Feb 28;60(3): M106-M131.













