August 1, 2022
By Yen H. Tran, MD, PhD, and Padmaja Sankaridurg, B.Optom, PhD, MIP
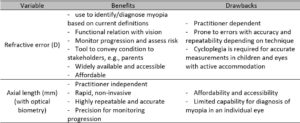
Both refractive error and axial length values have value in managing myopia. The tools enable the clinician to monitor an individual’s progress closely and accurately.

Management of myopia is becoming more imperative than before. In addition to the already high prevalence in many parts of the world, its prevalence is rising globally. It appears to have accelerated due to the restricted and indoor-based lifestyle brought about by the COVID pandemic.1,2 Fortunately, at present, there are many options to reduce the risk on onset as well as slow progression in eyes that are already myopic.
The efficacy of these options has been demonstrated in well-conducted, independent, prospective, randomized clinical trials.3 The outcomes of these trials were based on a difference in both changes in spherical equivalent refractive error and axial length between the myopia treatment strategies as compared to a control over a defined period. What exactly does that mean for the eye care practitioner who is trying to slow myopia in an individual in their practice? Should they consider change in refractive error alone, axial length alone, or both?
The Basics
Refractive error of the eye can be determined by several techniques ranging from subjective assessment to objective measurements using retinoscopy or autorefractors, either with or without cycloplegia. The accuracy and repeatability of refractive error measurements with these techniques vary, with subjective refraction providing the least repeatability of +/- 0.50D.4-6 Additionally, it is understood that especially in children and eyes where accommodation is active, non-cycloplegic assessments lead to a more myopic refractive error due to insufficient relaxation of accommodation.7 On the other hand, the newer generation of optical biometers that measure the antero-posterior distance between the corneal surface and the retinal pigment epithelium8 allow rapid measurements, are contactless, and proven to be more reliable and more precise than A-ultrasound with the resolution at 0.012mm and the precision at 0.01mm.8 Evidence also suggests that refraction and axial length changes are highly correlated.9 The mean repeatability of axial length measurements is +/- 0.12D and significantly higher than the mean of +/- 0.4D with cycloplegic auto-refraction and +/- 0.6D with non-cycloplegic auto-refraction.10
So, this brief look at the evidence may appear to support axial length measurements over refractive error measurements due to their accuracy and simplicity. However, it is not a case of simply favoring one over the other.
Firstly, we need refractive error measurements to diagnose myopia. Although there is progress in trying to understand the role of axial length measurements in screening/diagnosis of ametropia,11,12 presently, the information is insufficient to accurately categorize an eye as myopic. In this regard, cycloplegic refractive error continues to be the mainstay and the most accurate method to diagnose myopia, especially in young children. In addition, refractive error measurements also have a functional relationship with vision; the dioptric equivalents provide an indication of visual status. They can be used to monitor progression. Refractive error values are also used to explain the status of the eye and progression to parents/caregivers — a certain refractive error value indicates whether a child has poor vision at distance, near, or both. Then any changes can be used to determine progression.
Benefits of Axial Length Measurements
But when it comes to monitoring myopia progression, axial length measurements may be more valuable due to their higher accuracy/repeatability. Particularly, in those children receiving orthokeratology treatment, axial length measurements are possibly the only way to determine myopia progression. Axial length measurements also have value in categorizing the risk of an eye being myopic; higher axial length values (>25mm) indicate that the eye is at risk of having/developing myopia and indicate future risk of developing myopic maculopathy.13 Based on this understanding, in recent years, there has been the development of percentile /growth curves based on axial length — these population and gender-specific curves are used to determine the risk of development of myopia as well as the risk of progression.12,14,15 In addition, there are some developments to provide reference tables for categorizing progression as within normal/excessive range based on axial length.16
In summary, both refractive error and axial length values have value in managing myopia. The tools enable the clinician to monitor an individual’s progress closely and accurately. However, it is possible to practice myopia management even if one does not have access to all the tools. It is vital that myopia management is initiated as early as possible since progression appears to be rapid in younger children and especially in the years preceding and immediately after onset. Any increase in myopia increases the burden,17,18 and therefore, the focus should be on initiating treatment in an appropriate myopia management strategy.
 |
Prof. Padmaja Sankaridurg is Head, Myopia Program and Head, Intellectual Property at the Brien Holden Vision Institute and a Conjoint professor at the School of Optometry and Vision Science, Sydney, Australia. She also serves on the Advisory board of the International Myopia Institute and Review of Myopia Management. |
 |
Yen H. Tran, MD, PhD, Assoc. Prof., is the President of Hai Yen Vision Institute in Ho Chi Minh City, Vietnam, a leading translational research center in the field of myopia and refractive surgery in Vietnam. She has been collaborating with BHVI and other international entities over the years. |
References
- Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42.
- Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA ophthalmology. 2021;139(3):293-300.
- Wildsoet CF, Chia A, Cho P, Guggenheim JA, Polling JR, Read S, et al. IMI – Interventions Myopia Institute: Interventions for Controlling Myopia Onset and Progression Report. Investigative ophthalmology & visual science. 2019;60(3):M106-m31.
- Xiong S, Lv M, Zou H, Zhu J, Lu L, Zhang B, et al. Comparison of Refractive Measures of Three Autorefractors in Children and Adolescents. Optometry and vision science : official publication of the American Academy of Optometry. 2017;94(9):894-902.
- Pesudovs K, Weisinger HS. A comparison of autorefractor performance. Optometry and vision science : official publication of the American Academy of Optometry. 2004;81(7):554-8.
- Rosenfield M, Chiu NN. Repeatability of subjective and objective refraction. Optometry and vision science : official publication of the American Academy of Optometry. 1995;72(8):577-9.
- Sankaridurg P, He X, Naduvilath T, Lv M, Ho A, Smith E, 3rd, et al. Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta ophthalmologica. 2017;95(7):e633-e40.
- Wolffsohn JS, Kollbaum PS, Berntsen DA, Atchison DA, Benavente A, Bradley A, et al. IMI–Clinical myopia control trials and instrumentation report. Investigative ophthalmology&visual science. 2019;60(3):M132-M60.
- Fan Q, Wang H, Jiang Z. Axial length and its relationship to refractive error in Chinese university students. Contact Lens&Anterior Eye. 2022;45(2):101470.
- Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Progress in Retinal Eye Research. 2021;83:100923.
- He X, Zou H, Lu L, Zhao R, Zhao H, Li Q, et al. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PloS one. 2015;10(2):e0111766.
- He X, Sankaridurg P, Naduvilath T, Wang J, Xiong S, Weng R, et al. Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4-18 years. The British journal of ophthalmology. 2021.
- Hashimoto S, Yasuda M, Fujiwara K, Ueda E, Hata J, Hirakawa Y, et al. Association between axial length and myopic maculopathy: the Hisayama Study. Ophthalmology Retina. 2019;3(10):867-73.
- Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, et al. Axial length growth and the risk of developing myopia in European children. Acta ophthalmologica. 2018;96(3):301-9.
- Sanz Diez P, Yang LH, Lu MX, Wahl S, Ohlendorf A. Growth curves of myopia-related parameters to clinically monitor the refractive development in Chinese schoolchildren. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2019;257(5):1045-53.
- Chamberlain P, Lazon de la Jara P, Arumugam B, Bullimore MA. Axial length targets for myopia control. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2021;41(3):523-31.
- Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The Complications of Myopia: A Review and Meta-Analysis. Investigative ophthalmology & visual science. 2020;61(4):49.
- Sankaridurg P, Tahhan N, Kandel H, Naduvilath T, Zou H, Frick KD, et al. IMI Impact of Myopia. Investigative ophthalmology & visual science. 2021;62(5):2-.