Feb. 4, 2020
By Padmaja Sankaridurg, B.Opt, MIP, PhD
Brien Holden Vision Institute
The evidence for the rising prevalence of myopia and, therefore, its burden is irrefutable and substantial. In affected individuals, regular oversight is needed during the progression phase to restore visual acuity, and at higher levels of myopia, more frequent monitoring is required to detect and manage any associated complications. Although the condition stabilizes in early adulthood, in late adulthood, there is potential to develop complications especially in those with high myopia.
A number of strategies, both optical and pharmaceutical, slow the progression of myopia in comparison to single-vision spectacles and contact lenses. Employed appropriately, they reduce the risk of the eye attaining higher levels of myopia. However, in spite of the advances in myopia management, to date, single-vision spectacles or contact lenses continue to remain the most frequently used approach to manage myopia1. Clearly the process of managing any clinical condition is a complex decision that requires a careful assessment of risks versus benefits. Several factors may be responsible for the low uptake of myopia control strategies such as lack of sufficient and long term data on efficacy or safety of a particular strategy, practitioner skill base for a strategy, access to product, patient motivation, cost, convenience and acceptance, stable myopia, age of the individual and so on. While deliberating on the risks versus benefits for the newer myopia control options, it is also timely to weigh the risks versus benefits of continuing with single vision products. In this respect, there is an ongoing debate in the community on whether the use of single vision soft contact lenses and/or spectacles accelerate the progression of myopia.
Using a meta-analysis approach, annual myopia progression with single vision spectacles for a child of 9.3 years of age was estimated at -0.55D and -0.82D for European and Asian ethnicity, respectively. The estimated annual progression is less with increasing age and slightly higher in females.[2] In an unaided state, a myopic eye has myopic defocus, possibly more centrally than at the periphery based on the eye shape. When the eye is corrected with a single vision spectacle or contact lens, at the periphery, hyperopic defocus is observed. [3-5] It is widely believed and supported by data from animal models that myopic defocus slows eye growth, and hyperopic defocus either centrally and/or peripherally promotes progression.[6-9] Therefore, consistent with the model, fitting a myopic eye with a single vision product that results in peripheral hyperopia may result in accelerated progression. Furthermore, variation in the properties of optical devices (for example, pantoscopic tilt and power in the case of spectacles and aberrations, lens power, and power profile in the case of contact lenses) were reported to influence retinal defocus and suggested to affect progression variably.[10-14]
In trying to determine if single vision optical devices accelerate progression, an approach would be to compare and contrast the progression observed with single vision optical devices to that of progression in an unaided or an undercorrected eye.
In an interesting experiment, the dominant eyes of 11-year-old myopic children (-1.00 to -3.00D) were fully corrected, and the contralateral eyes left uncorrected or undercorrected. After 30 months, myopia progression in the uncorrected/undercorrected eye was slower by approximately 0.36D/year, resulting in anisometropia.[15] When the uncorrected/undercorrected eyes were refitted with single-vision spectacles, the eyes increased in progression and the induced anisometropia reduced. In another study, data of 121 grade 7 Chinese children (median age 12.7 yrs, 65 in the uncorrected and 56 fully corrected) were analyzed.[16] At two years, children with no correction had slower myopia progression (-0.76 ±1.04D versus -1.03±0.08D). The latter study had limitations with non-randomized groups and baseline differences that therefore raise queries on the validity of the results but both studies suggested that myopic defocus in the uncorrected or undercorrected eye resulted in less progression.
Although this may be construed as evidence for increased progression in fully corrected single vision lens wearing eyes, in other studies, bilateral under correction either resulted in worse progression or was no different compared to fully corrected eyes.[17, 18] Additionally, in another experiment, 68 Chinese children, 9-12 yrs of age, -0.50 to -3.50D were randomly assigned to either single-vision spectacles or no correction.[19] At the end of 12 months, change in SE/AL was -0.78 ±0.32/ 0.36 ±0.13mm in the no correction group versus -0.65±0.38/0.31 ±0.15mm in the corrected group and the difference not significant.
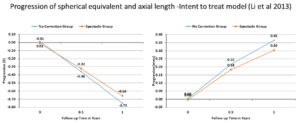
But there were some limitations with differences in baseline myopia (the no correction had lower baseline myopia as those with higher levels of myopia refused participation) and far more dropouts in the no correction group (11/33 versus 4/35). It is possible the dropouts were related to progression and vision in the uncorrected eyes.
In summary, understandably, there is limited information on the course of progression in an unaided myopic eye as when detected, the condition is corrected to restore sight. From the limited evidence, it is inconclusive that wearing single vision contact lenses or spectacles worsen myopia. Importantly undercorrection appears to have no role. But encouragingly, the evidence base for reduction of progression with optical and pharmaceutical strategies compared to single vision devices is strong and growing and provides the practitioner with several ways to better manage myopia.
- Wolffsohn, J.S., et al., Global trends in myopia management attitudes and strategies in clinical practice – 2019 Update. Cont Lens Anterior Eye, 2020. 43(1): p. 9-17.
- Donovan, L., et al., Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci, 2012. 89(1): p. 27-32.
- Chen, X., et al., Characteristics of peripheral refractive errors of myopic and non-myopic Chinese eyes. Vision research, 2010. 50(1): p. 31-35.
- Berntsen, D.A. and C.E. Kramer, Peripheral defocus with spherical and multifocal soft contact lenses. Optom Vis Sci, 2013. 90(11): p. 1215-24.
- Lin, Z., et al., Peripheral defocus with single-vision spectacle lenses in myopic children. Optom Vis Sci, 2010. 87(1): p. 4-9.
- Smith, E.L., 3rd, L.F. Hung, and J. Huang, Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res, 2009. 49(19): p. 2386-92.
- Wallman, J., et al., Local retinal regions control local eye growth and myopia. Science, 1987. 237(4810): p. 73-7.
- Hoogerheide, J., F. Rempt, and W.P. Hoogenboom, Acquired myopia in young pilots. Ophthalmologica, 1971. 163(4): p. 209-15.
- Hung, L.F., M.L. Crawford, and E.L. Smith, Spectacle lenses alter eye growth and the refractive status of young monkeys. Nat Med, 1995. 1(8): p. 761-5.
- Moore, K.E., J.S. Benoit, and D.A. Berntsen, Spherical Soft Contact Lens Designs and Peripheral Defocus in Myopic Eyes. Optom Vis Sci, 2017. 94(3): p. 370-379.
- De la Jara, P.L., Sankaridurg, P., Ho, A,, Martinez, A., Donovan, L., Smith, E.L., Chen, X., Ge, J., Holden, B., The Vision CRC Myopia Control Study Group, A silicone hydrogel contact lens produced less myopia progression than single vision spectacles in chinese children over a 6 month period. Investigative Ophthalmology and Vision Science, 2010. 51.
- Bakaraju, R.C., et al., Pantoscopic tilt in spectacle-corrected myopia and its effect on peripheral refraction. Ophthalmic Physiol Opt, 2008. 28(6): p. 538-49.
- Backhouse, S., et al., Peripheral refraction in myopia corrected with spectacles versus contact lenses. Ophthalmic Physiol Opt, 2012. 32(4): p. 294-303.
- Kwok, E., et al., Peripheral refraction in high myopia with spherical soft contact lenses. Optom Vis Sci, 2012. 89(3): p. 263-70.
- Phillips, J.R., Monovision slows juvenile myopia progression unilaterally. Br J Ophthalmol, 2005. 89(9): p. 1196-200.
- Sun, Y.Y., et al., Effect of uncorrection versus full correction on myopia progression in 12-year-old children. Graefes Arch Clin Exp Ophthalmol, 2017. 255(1): p. 189-195.
- Chung, K., N. Mohidin, and D.J. O’Leary, Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res, 2002. 42(22): p. 2555-9.
- Li, S.Y., et al., Effect of undercorrection on myopia progression in 12-year-old children. Graefes Arch Clin Exp Ophthalmol, 2015. 253(8): p. 1363-8.
- Li, L., et al., What is the ‘real’ baseline for the rate of progress of myopia for a child?The rate of progress of myopia with and without spectacle vision correction. Investigative Ophthalmology & Visual Science, 2013. 54(15): p. 5718-5718.

Padmaja Sankaridurg B.Opt, MIP, PhD, is the program Leader, Myopia and Manager, Intellectual Property at the Brien Holden Vision Institute in Sydney, Australia. She is also Conjoint Professor at the School of Optometry and Vision Science, University of New South Wales.













