September 1, 2020
By Rebecca Yan Shun Weng, BOptom (Hons), Grad Dip(I&T)
 The prevalence of myopia has increased dramatically, with an observable trend of earlier myopia onset in school-aged children.1,2 It is known that younger myopic children are prone to greater annual progression3,4, hence they are likely to progress to higher levels of myopia, leading to an increased risk of ocular complications if no intervention measure is implemented.5-7 A good myopia management plan starts with an accurate assessment of children’s vision, ocular health, binocular vision, and their refractive error status.
The prevalence of myopia has increased dramatically, with an observable trend of earlier myopia onset in school-aged children.1,2 It is known that younger myopic children are prone to greater annual progression3,4, hence they are likely to progress to higher levels of myopia, leading to an increased risk of ocular complications if no intervention measure is implemented.5-7 A good myopia management plan starts with an accurate assessment of children’s vision, ocular health, binocular vision, and their refractive error status.
In young children with active accommodation, a lack of cycloplegia will result in significant over-estimation of myopia, leading to a possible overcorrection of the condition or a failure to detect latent hyperopia. Autorefraction and subjective refraction performed under cycloplegia are much more precise than a non-cycloplegic ocular examination, minimizing chances of both over and under correction.
All children that present to the practice should undergo cycloplegic refraction. Several studies have demonstrated that eyes more likely to progress to myopia displayed an accelerated pattern of both refractive error and axial length growth a few years before the onset of myopia with the year before the first detection of myopia showing the greatest acceleration.8,9 The Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study found cycloplegic spherical equivalent refractive error the single best predictive risk factor for myopia onset. It concluded that a child with less hyperopia than the age norm is at greater risk for myopia development.9 The study proposed the following cut-off points to initiate preventative treatment9:
| Grade/Age | 6 years (Grade 1) | 7-8 years | 9-10 years | 11years |
| cut-off point to initiate preventative treatment | < +0.75D | ≤+0.50D | ≤ +0.25D | emmetropic |
Thus, it is the practitioner’s responsibility to assess and monitor refractive error of children using cycloplegia and offer preventative intervention to those who are bordering on the cut-off points or those displaying a trend of sudden acceleration in the direction of myopic refractive error. To date, an increase in time spent outdoors has been proven to be the evidence-based approach in reducing the incidence of myopia onset.10-12
For children who are already myopic, we need to establish a myopia management plan and decide on a treatment that we see as the most effective remedy. Once a treatment is chosen, it is necessary to utilize the same measurement procedure to ensure clinical data consistency. The IMI Clinical Management Guideline report recommends that “patients undergoing any myopia control treatment should be assessed at least every six months to monitor the safety and efficacy of treatment.”13 Hence a cycloplegic refraction should be performed at a minimum of every six months.
The standard of care to evaluate the effectiveness of the chosen treatment consists of both cycloplegic refractive error measurements and axial length measurements. The following two aspects should be considered when we are conducting the treatment efficacy assessment: 1) age normal progression rate and 2) expected treatment efficacy range.
Age Normal Progression Rate
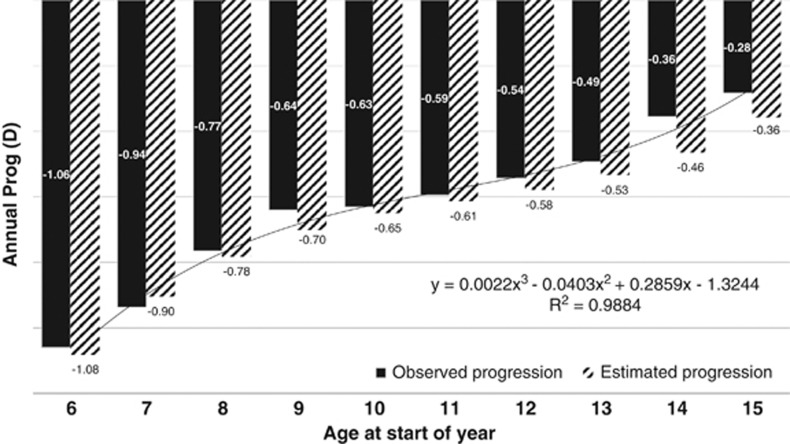
Several factors influence myopia progression rates with age being the most important one, an understanding of the age normal progression data allows us to compare them with our patient’s clinical data and assess treatment efficacy. Sankaridurg et al. analyzed data of 508 single vision spectacle wearers of Asian ethnicity. They estimated the annualized progression rate ranged from -0.36D to -1.08D for children aged 6-16 years old, showing a deceleration of progression rate with an increase in age (Figure 1).3 Furthermore, Donovan et al. conducted a meta-analysis of 20 studies of children wearing single vision spectacles for vision correction and derived the annual progression for 9 years old to be -0.55D and -0.82D, for Caucasians and Asians respectively.4 From these studies, it is safe to say that the annual progression rate for children wearing traditional optical correction (e.g., single vision spectacles), that is, without any intervention, ranges from -0.50D to -1.00D.
Figure 1. Annual progression data (observed and estimated) for children with myopia aged 6–12 years.3
Expected Treatment Efficacy Range
The treatment effect of each intervention method should also be well understood so that a realistic expectation outcome can be set with the chosen treatment. The IMI Clinical Management Guideline report summarized the efficacy range of the various treatment options with atropine treatment offering the most significant reduction in myopia progression ranging from 30 percent to 80 percent, followed by OrthoK lenses ranging from 30 percent to 60 percent, then multifocal or EDOF type soft contact lenses ranging from 30 percent to 50 percent, and lastly multifocal type or novel design spectacle lenses ranging from 20 percent to 50 percent.13 Also, almost all clinical studies demonstrate that the treatment effect is at its greatest in the first year.14,15 Hence, we need to factor this in when assessing the treatment efficacy and not to discourage patients from the myopia control treatment if they see a slowing down of treatment effects.
We need to include cycloplegic refraction as part of standard care for our myopic patients and those who are identified in the high-risk group. The use of cycloplegia enables us to manage myopia with an evidence-based approach. It provides us an accurate measurement that can be used for vision correction and helps us to identify pre-myopes so we can institute intervention timely to prevent and delay the myopia onset. Lastly, it allows us to evaluate myopia treatment efficacy with concrete data.
References
- Li SM, Liu LR, Li SY, et al. Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol 2013;20(6):348-59.
- Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt 2012;32(1):3-16.
- Sankaridurg PR, Holden BA. Practical applications to modify and control the development of ametropia. Eye (Lond) 2014;28(2):134-41.
- Donovan L, Sankaridurg P, Ho A, et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci 2012;89(1):27-32.
- Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology 2002;109(4):704-11.
- Xu L, Wang Y, Wang S, et al. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology 2007;114(2):216-20.
- Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt 2005;25(5):381-91.
- Xiang F, He M, Morgan IG. Annual changes in refractive errors and ocular components before and after the onset of myopia in Chinese children. Ophthalmology 2012;119(7):1478-84.
- Zadnik K, Sinnott LT, Cotter SA, et al. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol 2015;133(6):683-9.
- Wu PC, Tsai CL, Wu HL, et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013;120(5):1080-5.
- Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008;115(8):1279-85.
- He M, Xiang F, Zeng Y, et al. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China: A Randomized Clinical Trial. Jama 2015;314(11):1142-8.
- Gifford KL, Richdale K, Kang P, et al. IMI – Clinical Management Guidelines Report. Investigative Ophthalmology & Visual Science 2019;60(3):M184-M203.
- Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology 2006;113(12):2285-91.
- Cheng X, Brennan N, Toubouti Y. MODELLING OF CUMULATIVE TREATMENT EFFICACY IN MYOPIA PROGRESSION INTERVENTIONS2019.
Rebecca Yan Shun Weng, BOptom (Hons), is a Myopia Program Facilitator and Project Manager at the Brien Holden Vision Institute.