This summary of an International Myopia Institute (IMI) white paper was created by and is used with permission from the Centre for Ocular Research & Education (CORE) at the University of Waterloo’s School of Optometry & Vision Science in Waterloo, Ontario, Canada. It originally appeared in the April 2019 issue of Contact Lens Update, CORE’s free access online resource.
Myopia control is a growing area of clinical practice, with increased emphasis on early identification of risk factors and prescribing clinical interventions to slow the rate of progression. After extensive review of available evidence, this report provides guidelines on the management of myopes including baseline examination, treatment selection, ongoing management and patient/parental advice.
Baseline Exam
A comprehensive baseline exam identifies the risk factors for myopia, aids in the selection of treatment strategies, and establishes a benchmark to measure efficacy of treatments prescribed. The key elements of a baseline exam are outlined below:
Clinical Tests
- Appropriate history
- Distance and near VA
- Refraction
- Binocular vision tests
- Ocular health exam
If available, or on indication
- Axial Length measurement (every 6 months)
- Cycloplegic refraction (annually)
- Dilated fundus exam (annually)
Treatment specific tests:
- Atropine: pupil size and function, IOP
- Orthokeratology: corneal topography
Children younger than ten years old are expected to have mild levels of hyperopia. Lower hyperopia than age-normal can indicate risk of myopia development. Determining the phoria and accommodative functions help cater treatment modalities to the patient’s needs. Axial length and fundus examination can detect early indicators of pathological myopia. Structural changes in pathological myopia increases risk of developing retinal holes, tears or detachments, myopia maculopathy, glaucoma and cataract.
Treatment Strategies
Treatment selection
Multi-focal soft contact lenses (MFSCLs), orthokeratology (OK), atropine and progressive addition spectacle lenses (PALs) are all options to slow the rate of myopia progression. PALs have the most discrepancy in reported treatment effect and are generally reserved as a second-line treatment for those who are not suitable or ready for other methods.
Evidence supporting efficacy of MFSCL and OK is more consistent, but both are only available for a limited range of refractive errors, and generally cannot be fit for myopes with significant astigmatism. With these contact lens options, clinicians must determine whether children can safely self-administer and comply with lens wear.
Atropine may be contraindicated in some cases, and it may not be readily accessible, as it needs to be compounded by pharmacists at the most commonly prescribed doses in most coutries. Cost is another factor to be considered, as specialty contact lenses and additional appointments are required to manage these patients. Parents and eye care practitioners should work together to determine which modality may be best suited for a particular child.
Clinical care considerations
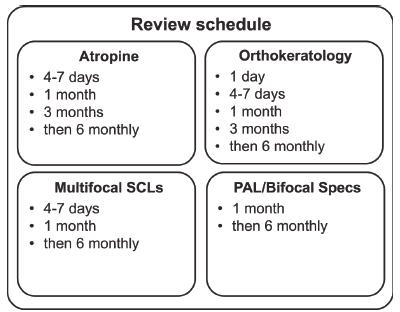
Generally, patients undergoing any myopia control treatment should be assessed at least every 6 months to monitor safety, compliance and treatment progress. The follow up schedule specific to each treatment is outlined in the figure below:
For patients who have significant astigmatism, in addition to the myopia control contact lenses, spectacles to correct residual astigmatism can be used. For patients on atropine, photochromic and PAL spectacles may be considered to alleviate the induced visual symptoms of the treatment. When prescribing MFSCL, practitioners need to consider which CL design to use, and if using presbyopic contact lenses off-label, need to select the appropriate add power, and counsel patients appropriately so they are fully informed of the off-label use.
Guidelines for Advice
Well-informed parents can be instrumental to the success of myopia management. Advice on key topics such as probable causes of myopia, dangers of high myopia, tools to help predict progression rate, near work vs outdoor activity, nutrition, when to end treatment and much more can be found in the full report, with a short summary available in the downloadable handout available in this issue of Contact Lens Update.
Other CORE summaries of IMI white papers
CORE’s Contact Lens Update, a free online resource