August 1, 2020
By Monica Jong, PhD, BOptom
 Myopia and high myopia are estimated to affect 50 percent (5 billion) and 10 percent (938 million) of the worldwide population by 2050, and consequently, we will also see a major increase in myopia-related vision impairment.1 Myopic macular degeneration is already a leading cause of permanent blindness in China, Taiwan, Japan, Netherlands, and Denmark.2 Higher levels of myopia are known to exponentially increase the risk of ocular complications such as retinal detachment, retinoschisis, open-angle glaucoma, and cataract, which may lead to permanent vision loss later in life.3 These are due to the abnormal increase in axial length in myopia4, leading to structural and physiological changes in the eye. Glaucoma is a chronic progressive optic neuropathy that is also a leading cause of permanent blindness worldwide5, and open-angle glaucoma is commonly reported in younger highly myopic patients6,7,8, hence there is a need to detect and treat early in these patients at risk.
Myopia and high myopia are estimated to affect 50 percent (5 billion) and 10 percent (938 million) of the worldwide population by 2050, and consequently, we will also see a major increase in myopia-related vision impairment.1 Myopic macular degeneration is already a leading cause of permanent blindness in China, Taiwan, Japan, Netherlands, and Denmark.2 Higher levels of myopia are known to exponentially increase the risk of ocular complications such as retinal detachment, retinoschisis, open-angle glaucoma, and cataract, which may lead to permanent vision loss later in life.3 These are due to the abnormal increase in axial length in myopia4, leading to structural and physiological changes in the eye. Glaucoma is a chronic progressive optic neuropathy that is also a leading cause of permanent blindness worldwide5, and open-angle glaucoma is commonly reported in younger highly myopic patients6,7,8, hence there is a need to detect and treat early in these patients at risk.
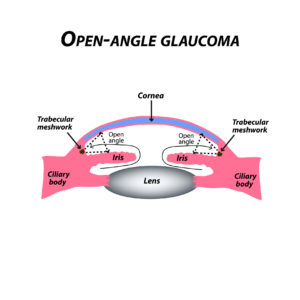
Open-angle glaucoma is a multifactorial disease, of which elevated intraocular pressure (IOP) is the most well known risk factor, along with ethnicity and familial history.9 The relation between myopia and open-angle glaucoma is not well understood. The underlying mechanism as to why myopia can lead to open-angle glaucoma is thought that the axial length increase leads to the tilting of the optic disc, causing damage to the axons in the lamina cribrosa.10 Studies have long ago identified myopia as a risk factor for developing open-angle glaucoma11,12,13, and in more recent times, studies such as the Beaver Dam Eye Study6, the Tajimi Study7, and Korean National Health and Nutrition Survey8 have reported a higher prevalence of glaucoma in highly myopic eyes compared to emmetropia. A retrospective study of high myopia reported 28 percent with open-angle glaucoma14, and most concerning, those individuals with open-angle glaucoma, were highly myopic and younger. The Korean population-based study8 also reported that younger participants (less than 40 years old) in the high-myopia group had higher open-angle glaucoma prevalence than the older participants (60+ years) in the lower myopia group.
A recent meta-analysis15 examined 14 population-based studies and reported that the overall odds ratio was 1.95 (95 percent confidence interval, 1.74 to 2.19) compared with emmetropia. For myopia up to -3D (low myopia), the odds ratio was 1.59 (95 percent confidence interval, 1.33-1.91), and for myopia -3D or worse (moderate/high myopia), the odds ratio was 2.92 (95 percent confidence interval, 1.89-4.52). Figure 1 (below) shows the individual odds ratio reported from each study and the overall pooled odds ratios for any myopia, low myopia, and moderate/high myopia. These findings are similar to an earlier meta-analysis on open-angle glaucoma and myopia.16
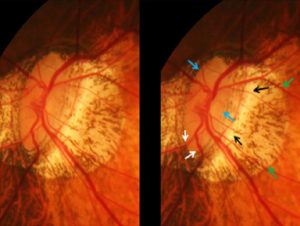
Distinguishing myopic optic neuropathy in high myopia from open-angle glaucoma can be difficult, leading to misdiagnosis. Highly myopic eyes tend to have larger optic disc sizes, more extensive excavations, enlarged parapapillary delta zone, be tilted, and not have a clear defined rim.17,18 Glaucomatous optic nerve damage (Figure 2 below) may be detected late in the course of the disease in those with high myopia because the IOP tends to be in the normal range.18 Given that a period of 20 years between diagnosis and perimetric blindness was estimated for open-angle glaucoma patients with average visual field loss progression9, early detection in our younger highly myopic patients is critical. Haarman et al15 has suggested optic-nerve screening at the age of 30 in myopic patients with spherical equivalent of refractive error –10D or worse, and at the age of 50 in patients with spherical equivalent of refractive error –6D to –10D.
Today, children as young as 6 are developing myopia and will likely become highly myopic.19 The risk of open-angle glaucoma and other ocular diseases in these individuals is real, and practitioners need to be aware to detect them in a younger population.
CONCLUSION
Myopia, and especially high myopia, increases the risk of open-angle glaucoma significantly. It is clear that there is a strong relationship between increased degree of myopia, patient age, and visual impairment.20,21 The more severe the myopia, the earlier the onset of sight-threatening complications.20,21 As practitioners, we need to be acutely aware of open-angle glaucoma in our patients who are young and highly myopic. It is vital to document optic-nerve-head changes using fundus photography, optical coherence tomography, and perimetry in our myopic patients to detect, diagnose, manage and prevent future permanent vision loss.
Figure 1. From Haarman et al 2020.15 Forest plot of OAG in any myopia (fixed effects model; Q = 8.3; I2 = 0.0); low myopia (fixed effects model; Q = 0.3; I2 = 0.0); category, which are as follows: any myopia OR, 1.95 (95% CI, 1.74–2.19); low myopia OR, 1.59 (95% CI, 1.33–1.91); moderate/high myopia and moderate/high myopia (random effects model; Q = 2.6; I2 = 0.0). Red lines with diamond represents the summary OR per myopia OR, 2.92 (95% CI, 1.89–4.52).
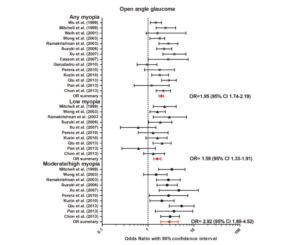
Figure 2. Image from Jonas et al14 Stereoscopic photograph of a glaucomatous optic nerve head in a highly myopic eye with parapapillary gamma zone (green arrows), parapapillary delta zone (black arrows), and retinal vessel kinking close to the optic disc border (white arrows); blue arrows: optic disc border (peripapillary ring).
REFERENCES
- Holden, B. A. et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology (2016) doi:10.1016/j.ophtha.2016.01.006.
- Fricke, T. R. et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol 102, 855–862 (2018).
- Flitcroft, D. I. Progress in Retinal and Eye Research. The complex interactions of retinal, optical, and environmental factors in myopia aetiology. Prog. Retin. Eye Res. 31, 622–660 (2012).
- Tideman, J. W. L. et al. Association of axial length with risk of uncorrectable visual impairment for europeans with myopia. JAMA Ophthalmol. 134, 1355–1363 (2016).
- Flaxman, S. R. et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob. Heal. 5, e1221–e1234 (2017).
- Wong, T. Y., Klein, B. E. K., Klein, R., Knudtson, M. & Lee, K. E. Refractive errors, intraocular pressure, and glaucoma in a white population. Ophthalmology 110, 211–217 (2003).
- Suzuki, Y. et al. Risk Factors for Open-Angle Glaucoma in a Japanese Population. The Tajimi Study. Ophthalmology 113, 1613–1617 (2006).
- Shim, S. H. et al. The Prevalence of Open-Angle Glaucoma by Age in Myopia: The Korea National Health and Nutrition Examination Survey. Curr Eye Res 42, 65–71 (2017).
- Saunders, L. J., Medeiros, F. A., Weinreb, R. N. & Zangwill, L. M. What rates of glaucoma progression are clinically significant? Expert Review of Ophthalmology vol. 11 227–234 (2016).
- Doshi, A., Kreidl, K. O., Lombardi, L., Sakamoto, D. K. & Singh, K. Nonprogressive Glaucomatous Cupping and Visual Field Abnormalities in Young Chinese Males. Ophthalmology 114, 472–479 (2007).
- Perkins, E. S. & Phelps, C. D. Open Angle Glaucoma, Ocular Hypertension, Low-Tension Glaucoma, and Refraction. Arch. Ophthalmol. 100, 1464–1467 (1982).
- Knapp, A. Glaucoma in myopic eyes. Trans Am Ophthalmol Soc 61–70. (1925).
- Daubs, J. G. & Crick, R. P. Effect of refractive error on the risk of ocular hypertension and open-angle glaucoma. Trans. Ophthalmol. Soc. U. K. 101, 121–126 (1981).
- Jonas, J. B., Weber, P., Nagaoka, N. & Ohno-Matsui, K. Glaucoma in high myopia and parapapillary delta zone. PLoS One 12, e0175120 (2017).
- Haarman, A. E. G. et al. The Complications of Myopia: A Review and Meta-Analysis. Invest. Ophthalmol. Vis. Sci. 61, 49 (2020).
- Marcus, M. W., De Vries, M. M., Junoy Montolio, F. G. & Jansonius, N. M. Myopia as a risk factor for open-angle glaucoma: A systematic review and meta-analysis. Ophthalmology 118, 1989-1994.e2 (2011).
- Jagadeesh, D. et al. Posterior segment conditions associated with myopia and high myopia. Clin. Exp. Optom. 1–10 (2020) doi:10.1111/cxo.13060.
- Jonas, J. B., Panda-Jonas, S. & Ohno-Matsui, K. Glaucoma in high myopia. in Updates on Myopia: A Clinical Perspective 241–255 (Springer Singapore, 2019). doi:10.1007/978-981-13-8491-2_11.
- Sankaridurg, P. R. & Holden, B. A. Practical applications to modify and control the development of ametropia. Eye 28, 134–141 (2014).
- Tideman, J. W. L., Polling, J. R., Jaddoe, V. W. V., Vingerling, J. R. & Klaver, C. C. W. Environmental Risk Factors Can Reduce Axial Length Elongation and Myopia Incidence in 6- to 9-Year-Old Children. Ophthalmology 126, 127–136 (2019).
- Verhoeven, V. J. M. et al. Visual consequences of refractive errors in the general population. Ophthalmology 122, 101–109 (2015).

Monica Jong, PhD, BOptom, is Executive Director, International Myopia Institute; Assistant Professor, Discipline of Optometry and Vision Science, University of Canberra, Australia; Visiting Fellow, Brien Holden Vision Institute, Sydney; and Visiting Fellow, School of Optometry and Vision Science, UNSW Sydney.