April 12, 2019
By Jennifer Sha, BOptom, BSc(Hons), Senior Research Optometrist
Brien Holden Vision Institute
 By 2020 the global prevalences of myopia and high myopia are estimated to be 34% and 5.2%, respectively and are predicted to increase.1 Due to the increased risk of developing associated complications such as retinal detachment, glaucoma, cataract, and myopic macular degeneration, as well as the burden to society, much effort has been made in recent decades to understand myopia progression and methods of slowing its progression.
By 2020 the global prevalences of myopia and high myopia are estimated to be 34% and 5.2%, respectively and are predicted to increase.1 Due to the increased risk of developing associated complications such as retinal detachment, glaucoma, cataract, and myopic macular degeneration, as well as the burden to society, much effort has been made in recent decades to understand myopia progression and methods of slowing its progression.
Emmetropization is the process that occurs during childhood and adolescence whereby the axial length of the eye is regulated to closely match the refractive power.2 Most infants are hyperopic, and while emmetropization reduces the refractive error, children typically converge to a low level of hyperopia by teen years.3 However, emmetropization does not always proceed in this manner, and in children who become myopic, axial length is longer and refractive error is less hyperopic than normal for up to 3 years before even the onset of myopia.4 With respect to the level of refractive error that is considered abnormal, the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study demonstrated that 6 year old children with refraction ≤+0.75D were at an increased risk of developing myopia, as well as 7-8 year old children with ≤+0.50D, 9-10 year old children with ≤+0.25D, and 11 year old children with ≤0.00D.5
Research has uncovered some characteristics of people at greater risk of developing myopia. These include at least one parent with myopia,6, 7 female gender,8-10 very close reading distances and longer continuous reading time.11, 12 Age is an interesting risk factor, as the prevalence of myopia is higher in older children,6 while the progression rate is greater in younger children.13, 14 Myopic children may also exhibit more esophoria,15 more accommodative lag,16 reduced accommodative facility,17 and a greater AC/A ratio,18 however it is not clear whether these binocular vision features are a cause or an effect of the myopia.
In terms of ethnicity, myopia prevalence is significantly higher in East Asian children compared to Caucasian children even in the same geographic location.6, 8, 19 Not only that; myopia progression is higher in Asian children compared to Caucasian children. A meta-analysis of studies reporting myopia progression in children wearing spectacles estimated that rates of progression were -0.55D per year for Caucasian children and -0.82D per year for Asian children with the same degree of myopia at 9 years of age.20 Progression was faster for Asians compared to Caucasians at every time point over 3 years. However, it is not completely clear if these ethnicity differences are due to genetic factors, environmental factors, or both as East Asian children also spend less time outdoors on average than their Caucasian counterparts,6 which is also a risk factor for developing myopia.21
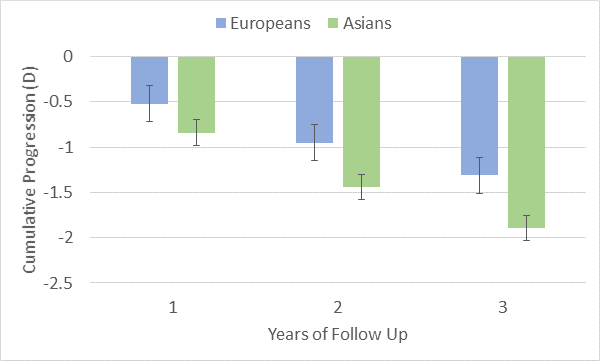
Estimated cumulative myopia progression for European and Asian children over 1-3 years of follow up reported by Donovan, et al. (2012). Error bars indicate 2x the standard error.
Clearly, the more risk factors present, the greater the onus to discuss myopia management with both child and parent. Evaluation should begin with comparing refraction and age against the guidelines reported by the CLEERE study. For children not yet myopic but less hyperopic than these guidelines, discussing outdoor time and reading habits is prudent as behavioural changes may be easily implemented with few downsides, and may prevent the onset of myopia. Going a step further, these actions could even be recommended to all children, myopic or not, as there is no harm (so long as they are sensible with sun protection).
Once myopia has already developed, beginning other forms of myopia management (optical, pharmaceutical, or both) to slow myopia progression is advisable,22 particularly for younger children, as they will likely have more years of progression and therefore may have a higher net myopia. Hence, earlier intervention will reduce the risk of the child developing high myopia and the associated complications later in life. The risk of progression and intervention strategies should be discussed with parents/carers. Some parents, particularly those who are myopic themselves, may be more willing to intervene at an earlier stage.
The age of the child and level of myopia will also influence the form of management. For young children in the early stages of developing myopia, choosing a strategy that befits the age, that are easily implementable and have a good safety profile is advisable (for example, a spectacle based strategy over contact lenses or pharmaceutical approaches), whereas for those with higher levels of myopia and faster progression, a pharmaceutical strategy or combination of pharmaceutical and optical may be more appropriate. At the very least, myopic children need to keep their prescriptions as up-to-date as possible, as undercorrection increases the rate of progression.23
In summary, currently, a number of myopia management strategies are available. For long term success, a number of factors related to the risk profile of the patient and their carer, their enthusiasm and motivation for myopia control strategies as well as clinical judgment of eye care practitioners having considered their ocular health will dictate the type of myopia management strategy.
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036-42.
- Wildsoet CF. Active Emmetropization – Evidence for Its Existence and Ramifications for Clinical Practice. Ophthal Physiol Opt 1997;17:279-90.
- Flitcroft DI. Emmetropisation and the Aetiology of Refractive Errors. Eye 2014;28:169-79.
- Mutti DO, Hayes JR, Mitchell GL, et al. Refractive Error, Axial Length, and Relative Peripheral Refractive Error before and after the Onset of Myopia. Invest Ophthalmol Vis Sci 2007;48:2510-9.
- Zadnik K, Sinnott LT, Cotter SA, et al. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol 2015;133:683-9.
- French AN, Morgan IG, Mitchell P, Rose KA. Risk Factors for Incident Myopia in Australian Schoolchildren: The Sydney Adolescent Vascular and Eye Study. Ophthalmology 2013;120:2100-8.
- Jones LA, Sinnott LT, Mutti DO, et al. Parental History of Myopia, Sports and Outdoor Activities, and Future Myopia. Invest Ophthalmol Vis Sci 2007;48:3524-32.
- Ip JM, Huynh SC, Robaei D, et al. Ethnic Differences in Refraction and Ocular Biometry in a Population-Based Sample of 11-15-Year-Old Australian Children. Eye 2008;22:649-56.
- Sun J, Zhou J, Zhao P, et al. High Prevalence of Myopia and High Myopia in 5060 Chinese University Students in Shanghai. Invest Ophthalmol Vis Sci 2012;53:7504-9.
- Matamoros E, Ingrand P, Pelen F, et al. Prevalence of Myopia in France. Medicine 2015;94:e1976.
- Ip JM, Saw SM, Rose KA, et al. Role of near Work in Myopia: Findings in a Sample of Australian School Children. Invest Ophthalmol Vis Sci 2008;49:2903-10.
- Li SM, Li SY, Kang MT, et al. Near Work Related Parameters and Myopia in Chinese Children: The Anyang Childhood Eye Study. PloS One 2015;10:e0134514.
- Price H, Allen PM, Radhakrishnan H, et al. The Cambridge Anti-Myopia Study: Variables Associated with Myopia Progression. Optom Vis Sci 2013;90:1274-83.
- Sankaridurg P, Holden BA. Practical Applications to Modify and Control the Development of Ametropia. Eye 2014;28:134-41.
- Drobe B, Saint-André D. The Pre-Myopic Syndrome. Ophthalmic Physiol Opt 1995;15:375-8.
- Nakatsuka C, Hasebe S, Nonaka F, Ohtsuki H. Accommodative Lag under Habitual Seeing Conditions: Comparison between Myopic and Emmetropic Children. Jpn J Ophthalmol 2005;49:189-94.
- Pandian A, Sankaridurg PR, Naduvilath T, et al. Accommodative Facility in Eyes with and without Myopia. Invest Ophthalmol Vis Sci 2006;47:4725-31.
- Gwiazda J, Thorn F, Held R. Accommodation, Accommodative Convergence, and Response Ac/a Ratios before and at the Onset of Myopia in Children. Optom Vis Sci 2005;82:273-8.
- Rudnicka AR, Owen CG, Nightingale CM, et al. Ethnic Differences in the Prevalence of Myopia and Ocular Biometry in 10- and 11-Year-Old Children: The Child Heart and Health Study in England (Chase). Invest Ophthalmol Vis Sci 2010;51:6270-6.
- Donovan L, Sankaridurg P, Ho A, et al. Myopia Progression Rates in Urban Children Wearing Single-Vision Spectacles. Optom Vis Sci 2012;89:27-32.
- Xiong S, Sankaridurg P, Naduvilath T, et al. Time Spent in Outdoor Activities in Relation to Myopia Prevention and Control: A Meta-Analysis and Systematic Review. Acta Ophthalmol 2017;95:551-66.
- Michaud L, Simard P, Marcotte-Collard R. Defining a Strategy for Myopia Control. Contact Lens Spectrum 2016;31:36-42.
- Vasudevan B, Esposito C, Peterson C, et al. Under-Correction of Human Myopia – Is It Myopigenic?: A Retrospective Analysis of Clinical Refraction Data. J Optom 2014;7:147-52.













