Sponsored content
By Jonathan Skoner, OD, FIAOMC
Troubleshooting in Ortho-K is best done when all of the crucial decision-making information is obtained for every visit. Critical follow-up information includes:
- History taking
- Topography
- Refraction
- Slit lamp exam and fluorescein (FL) pattern assessment
History Taking: Use patient history to understand if your clinical results will be accurate or skewed in some way. Understand what time the patient took out the lenses in the morning, how long they slept with them, and how many consecutive nights the current set of lenses have been worn. These are all important factors that will directly impact the results you see in the exam room.
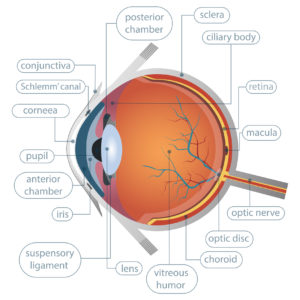
Topography: Topography is critical to assess the changes that are made to the cornea overnight in a closed eye environment; it is the standard of care. The most critical topographical assessments come from the difference (subtractive) maps (both tangential and axial) using a good baseline image. Be sure to use the tangential map to assess centration of lens overnight (along with centration of treatment zone) and watch for central islands. Axial maps are best used for determining initial corneal astigmatism and treatment zone size/location.
Refraction: Refraction can be tricky on an Ortho-K patient, as auto-refraction often yields erroneous values. It is good practice to use the difference in axial and refractive topography maps to get an estimate of how much the prescription has changed in diopters on the visual axis from baseline.
Slit Lamp Exam and FL Pattern Assessment: Use this to check corneal integrity after wearing lenses overnight. Ensure that the epithelial health is proper without staining or other adverse effects. The FL lens pattern will help you determine apical clearance, tear exchange and peripheral corneal alignment.
Troubleshooting Corneal Topographies
High Riding: This is typically caused by a lens fit that is too “flat” and the sagital depth is too shallow.
Adjustment: Steepen the overall lens fit by increasing sagital depth, most easily done by steepening alignment curve(s) (AC). Ensure proper lens diameter. Too small of a lens will have an insufficient balance of (centration, push/pull) forces and ineffective sized AC(s).
Low Riding: This fit usually indicates the sagital depth of the lens is too deep, referred to as a “steep” fit.
Adjustment: Flatten the overall lens fit by decreasing sagital depth, most easily done by flattening AC(s). Again, proper diameter is very important to allow AC(s) to do their job.
Lateral Decentration: This can be caused by multiple issues, most commonly a diameter that is too small, a steep/flat fitting lens, or a toric cornea with improperly fit AC(s).
Adjustment: Ensure the diameter is 95-97% of HVID (be mindful of VVID). Use FL pattern to determine if AC(s) are too steep or too flat and adjust accordingly, topography can be misleading for this assessment. Add toricity to AC(s) if the lens shows lift-off on the FL pattern. This can work very well for helping lateral decentration. Check the lens surface for deposits, and perform a deep clean with progent in office, if needed. In some cases after all other options are tried, depending on pre-fit peripheral corneal irregularity (reference your baseline measurements), decreasing the lens diameter to smaller than average can also be a fix.
Central Island: Use the difference in topography maps and refraction to ensure true central island is present and it’s not a false central island or corneal staining from an epithelial insult. Usually a steep-fitting lens with excessive sagital depth causes a true central island.
Adjustment: Flatten the overall lens fit by decreasing sagital depth. Evaluate your AC(s) and reverse curve(s) (RC) in the FL pattern to determine which may need adjustment.
Induced Astigmatism/Dimple Veiling: This is usually caused by a steep or tight-fitting lens.
Adjustment: Observe FL pattern to determine the best way to loosen fit on cornea. Best methods usually include flattening AC(s), lower the apical clearance of the lens by flattening the RC(s) or adding toricity to allow a more relaxed corneal/lens relationship 360 degrees.
Lastly, talk with consultants from the companies of the various lenses you work with. These consultants have fit thousands of lenses and are truly the best source to learn specifics to each lens design. Ask questions on their decision making and suggested changes as they explain their reasoning. It will reinforce your knowledge base.

Jonathan Skoner, OD, FIAOMC, is founder of Ortho Eyes, in McMurray, PA. Contact: drskoner@orthoeyes.com
 |
||
| The Ortho-K Knowledge Bank provides clinical insights and strategies for practice management and business growth. It is created by Review of Optometric Business and Review of Myopia Management for sponsor GP Specialists. | ||
 |
 |
 |