June 8, 2020
By Xiaoying Zhu, OD, PhD, MD, MS, FAAO
 Myopia is currently a major public health concern because of its rapidly increasing prevalence worldwide and the threat to vision. It has been estimated that 50 percent of the world population will be myopic in 2050, with 10 percent having high myopia.1 Myopia can cause a wide spectrum of complications, such as cataracts, glaucoma, retinal detachment, and myopia maculopathy. As a result, the World Health Organization recognizes that myopia, if not fully corrected, is a significant cause of visual impairment.2
Myopia is currently a major public health concern because of its rapidly increasing prevalence worldwide and the threat to vision. It has been estimated that 50 percent of the world population will be myopic in 2050, with 10 percent having high myopia.1 Myopia can cause a wide spectrum of complications, such as cataracts, glaucoma, retinal detachment, and myopia maculopathy. As a result, the World Health Organization recognizes that myopia, if not fully corrected, is a significant cause of visual impairment.2
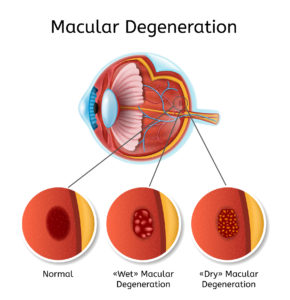
Myopic maculopathy (MM), also known as myopic macular degeneration, is the most serious, irreversible, vision-threatening complication and the leading cause of bilateral visual impairment and blindness.3-8 Fricke et al. reported that in 2015 MM caused visual impairment in 10 million people and blindness in 3.3 million people worldwide.9 It is estimated that, without changing the current interventions, up to 55.7 million people will have visual impairment, and up to 18.5 million people will be blind, due to MM in 2050.
MM poses a tremendous burden to patients, their families, and society. Naidoo et al. reported the global productivity loss caused by MM to be $6 billion.10 With the speculation that half of the world population will be myopic in 20501, it is conceivable that this financial burden will worsen in the near future.
These most recent findings on MM review its prevalence, risk factors, clinical presentations (categories), prevention, and treatment.
Prevalence
The prevalence of MM ranged from 0.2 percent to 4.0 percent in myopic patients.11 Specifically, the prevalence varied from 13.3 percent to 65.4 percent in high myopes, 0.3 percent to 7.8 percent in moderate myopes, and 0.1 percent to 7.0 percent in low myopes.12-19 Furthermore, Haarman et al. conducted a meta-analysis on eight population-based studies and reported significantly increased odds ratio (OR) values for myopia (OR: 102 with all levels of myopia pooled, 845, 73, and 14 for high, moderate, and low myopia, respectively). Therefore, while MM is more commonly seen in high myopic patients, moderate and even low myopia also significantly increase the risk of myopia maculopathy.20
Risk Factors
Not surprisingly, higher refractive error18,21-23 and longer axial length18,24,25 carry higher risks for MM. Hashimoto et al. reported in a Japanese population that the optimal cutoff values for identifying MM were 25.9 mm and 25.3 mm in men and women, respectively. Compared with patients with axial lengths below these values, patients with axial lengths above these values showed a significantly higher OR of MM (men: 21, women: 38).24 Bikbov et al. also found that a higher MM prevalence was associated with longer axial length (OR, 4.54) in a Russian population-based study.25
In addition, older age,12,13,18,21,25-27 reduced choroidal thickness,28 and posterior staphyloma29,30 are also considered to be risk factors for MM. On the other hand, MM does not seem to be associated with any major internal medical disease or level of education.25
Clinical Presentations
MM is one of the earliest complications associated with myopia. It comprises stretched blood vessels, peripapillary atrophy, posterior staphyloma, diffuse, patchy macular atrophy with or without lacquer cracks, subretinal hemorrhages, choroidal neovascularization (CNV), Fuch’s spot, and chorioretinal atrophy.29 As mentioned above, MM irreversibly reduces BCVA.11 Indeed, macular atrophy had the most significant impact on BCVA, followed by CNV, patchy atrophy, diffuse atrophy, or lacquer cracks.31 Tessellated fundus, in contrast, did not affect BCVA. It has also been shown that patients with macular atrophy, CNV, or Fuchs spot had worse BCVA compared with those with patchy or diffuse atrophy, lacquer cracks, or tessellated fundus.11
MM can be classified in the following five categories based on the International Photographic Classification and Grading System:29
Category 0: no myopic retinal degenerative lesion
Category 1: tessellated fundus
Category 2: diffuse chorioretinal atrophy
Category 3: patchy chorioretinal atrophy
Category 4: macular atrophy
Note that lacquer cracks, CNV, and Fuch’s spot are considered to be the “plus” lesions.
Prevention/Treatment
Unfortunately, there is no established treatment for MM at this point. However, the key is that preventative therapy aiming to reduce ocular complications should be considered for all myopic patients. Bullimore et al. estimated that each 1 diopter increase in myopia is associated with a 67 percent increase of myopic maculopathy and that slowing myopia progression by 1 diopter should reduce the likelihood of MM by 40 percent.20 As such, it is fundamental to reduce myopia onset and progression to prevent future ocular complications. The current consensus for patients with progressive myopia and risk factors for faster myopia progression is that they should be put on myopia control (orthokeratology, multifocal contact lenses, low dose atropine, and bifocal glasses/progressive addition lenses) and monitored twice a year.32,33 Those with high myopia should be monitored even more closely due to the higher risks of developing ocular complications, including myopic CNV, and referred to treatment if indicated.
While there is no established treatment for MM, the current treatment options are similar to those for age-related macular disease (AMD) and are cause-specific. Intravitreal injection of anti-VEGF (e.g., bevacizumab) is the first-line treatment for myopic CNV, which can improve the mean visual acuity by two to five lines after two years,34 but not after four years of treatment,35,36 probably due to CNV-related macular atrophy. Compared to those with wet AMD, patients with myopic CNV require fewer injections on average with better visual outcomes. Laser and surgical interventions have also been used to treat myopic CNV but only yield limited effects.37 Furthermore, vitrectomy may be required to treat a macular hole caused by MM.
Patients with MM can also benefit from low-vision aids, such as high-addition monofocal, bifocal, or trifocal lenses, as well as hand-held or self-standing magnification systems.
Xiaoying Zhu, OD, MD, PhD, MS, FAAO, is an Assistant Clinical Professor and Director of the Myopia Control Clinic at the State University of New York College of Optometry.
References:
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036-42.
- Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet 2012;379:1739-48.
- Xu L, Wang Y, Li Y, et al. Causes of Blindness and Visual Impairment in Urban and Rural Areas in Beijing: The Beijing Eye Study. Ophthalmology 2006;113:1134 e1-11.
- Hsu WM, Cheng CY, Liu JH, et al. Prevalence and Causes of Visual Impairment in an Elderly Chinese Population in Taiwan: The Shihpai Eye Study. Ophthalmology 2004;111:62-9.
- Dineen B, Bourne RR, Jadoon Z, et al. Causes of Blindness and Visual Impairment in Pakistan. The Pakistan National Blindness and Visual Impairment Survey. Br J Ophthalmol 2007;91:1005-10.
- Liang YB, Friedman DS, Wong TY, et al. Prevalence and Causes of Low Vision and Blindness in a Rural Chinese Adult Population: The Handan Eye Study. Ophthalmology 2008;115:1965-72.
- Gunnlaugsdottir E, Arnarsson A, Jonasson F. Prevalence and Causes of Visual Impairment and Blindness in Icelanders Aged 50 Years and Older: The Reykjavik Eye Study. Acta Ophthalmol 2008;86:778-85.
- Zheng Y, Lavanya R, Wu R, et al. Prevalence and Causes of Visual Impairment and Blindness in an Urban Indian Population: The Singapore Indian Eye Study. Ophthalmology 2011;118:1798-804.
- Fricke TR, Jong M, Naidoo KS, et al. Global Prevalence of Visual Impairment Associated with Myopic Macular Degeneration and Temporal Trends from 2000 through 2050: Systematic Review, Meta-Analysis and Modelling. Br J Ophthalmol 2018;102:855-62.
- Naidoo KS, Fricke TR, Frick KD, et al. Potential Lost Productivity Resulting from the Global Burden of Myopia: Systematic Review, Meta-Analysis, and Modeling. Ophthalmology 2019;126:338-46.
- Haarman AEG, Enthoven CA, Tideman JWL, et al. The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthal Vis Sci 2020;61:49.
- Vongphanit J, Mitchell P, Wang JJ. Prevalence and Progression of Myopic Retinopathy in an Older Population. Ophthalmology 2002;109:704-11.
- Liu HH, Xu L, Wang YX, et al. Prevalence and Progression of Myopic Retinopathy in Chinese Adults: The Beijing Eye Study. Ophthalmology 2010;117:1763-8.
- Gao LQ, Liu W, Liang YB, et al. Prevalence and Characteristics of Myopic Retinopathy in a Rural Chinese Adult Population: The Handan Eye Study. Arch Ophthalmol 2011;129:1199-204.
- Asakuma T, Yasuda M, Ninomiya T, et al. Prevalence and Risk Factors for Myopic Retinopathy in a Japanese Population: The Hisayama Study. Ophthalmology 2012;119:1760-5.
- Chen SJ, Cheng CY, Li AF, et al. Prevalence and Associated Risk Factors of Myopic Maculopathy in Elderly Chinese: The Shihpai Eye Study. Invest Ophthal Vis Sci 2012;53:4868-73.
- Jonas JB, Nangia V, Gupta R, et al. Prevalence of Myopic Retinopathy in Rural Central India. Acta Ophthalmol 2017;95:e399-e404.
- Choudhury F, Meuer SM, Klein R, et al. Prevalence and Characteristics of Myopic Degeneration in an Adult Chinese American Population: The Chinese American Eye Study. Am J Ophthalmol 2018;187:34-42.
- Wong YL, Sabanayagam C, Ding Y, et al. Prevalence, Risk Factors, and Impact of Myopic Macular Degeneration on Visual Impairment and Functioning among Adults in Singapore. Invest Ophthal Vis Sci 2018;59:4603-13.
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5.
- Hopf S, Korb C, Nickels S, et al. Prevalence of Myopic Maculopathy in the German Population: Results from the Gutenberg Health Study. Br J Ophthalmol 2019.
- Xiao O, Guo X, Wang D, et al. Distribution and Severity of Myopic Maculopathy among Highly Myopic Eyes. Invest Ophthal Vis Sci 2018;59:4880-5.
- Yu X, Ma W, Liu B, et al. Morphological Analysis and Quantitative Evaluation of Myopic Maculopathy by Three-Dimensional Magnetic Resonance Imaging. Eye (Lond) 2018;32:782-7.
- Hashimoto S, Yasuda M, Fujiwara K, et al. Association between Axial Length and Myopic Maculopathy: The Hisayama Study. Ophthalmol Retina 2019;3:867-73.
- Bikbov MM, Gilmanshin TR, Kazakbaeva GM, et al. Prevalence of Myopic Maculopathy among Adults in a Russian Population. JAMA Netw Open 2020;3:e200567.
- Hsiang HW, Ohno-Matsui K, Shimada N, et al. Clinical Characteristics of Posterior Staphyloma in Eyes with Pathologic Myopia. Am J Ophthalmol 2008;146:102-10.
- Li Z, Liu R, Jin G, et al. Prevalence and Risk Factors of Myopic Maculopathy in Rural Southern China: The Yangxi Eye Study. Br J Ophthalmol 2019;103:1797-802.
- Koh V, Tan C, Tan PT, et al. Myopic Maculopathy and Optic Disc Changes in Highly Myopic Young Asian Eyes and Impact on Visual Acuity. Am J Ophthalmol 2016;164:69-79.
- Ohno-Matsui K, Kawasaki R, Jonas JB, et al. International Photographic Classification and Grading System for Myopic Maculopathy. Am J Ophthalmol 2015;159:877-83 e7.
- Yan YN, Wang YX, Yang Y, et al. Ten-Year Progression of Myopic Maculopathy: The Beijing Eye Study 2001-2011. Ophthalmology 2018;125:1253-63.
- Hayashi K, Ohno-Matsui K, Shimada N, et al. Long-Term Pattern of Progression of Myopic Maculopathy: A Natural History Study. Ophthalmology 2010;117:1595-611, 611 e1-4.
- Wildsoet CF, Chia A, Cho P, et al. Imi – Interventions Myopia Institute: Interventions for Controlling Myopia Onset and Progression Report. Invest Ophthal Vis Sci 2019;60:M106-M31.
- Gifford KL, Richdale K, Kang P, et al. Imi – Clinical Management Guidelines Report. Invest Ophthal Vis Sci 2019;60:M184-M203.
- Lai TY, Luk FO, Lee GK, Lam DS. Long-Term Outcome of Intravitreal Anti-Vascular Endothelial Growth Factor Therapy with Bevacizumab or Ranibizumab as Primary Treatment for Subfoveal Myopic Choroidal Neovascularization. Eye (Lond) 2012;26:1004-11.
- Oishi A, Yamashiro K, Tsujikawa A, et al. Long-Term Effect of Intravitreal Injection of Anti-Vegf Agent for Visual Acuity and Chorioretinal Atrophy Progression in Myopic Choroidal Neovascularization. Graefes Arch Clin Exp Ophthalmol 2013;251:1-7.
- Ruiz-Moreno JM, Montero JA, Araiz J, et al. Intravitreal Anti-Vascular Endothelial Growth Factor Therapy for Choroidal Neovascularization Secondary to Pathologic Myopia: Six Years Outcome. Retina 2015;35:2450-6.
- Silva R. Myopic Maculopathy: A Review. Ophthalmologica 2012;228:197-213.













