February 7, 2019
By Tim Fricke, BOptom, MSc
Brien Holden Vision Institute
 Eye care practitioners see the burden of myopia in individuals every day: patients worrying about refractive changes; patients needing to update glasses and/or contact lenses to recover vision lost to myopia progression; patients with myopia-associated pathology and/or vision loss from those conditions; parents who worry about their children becoming myopic and progressing to higher levels of myopia, etc. These personal burdens also have some community-level implications via their effect on health expenditure, quality of life and productivity. However, the significant public health implications of myopia and high myopia are ones that clinical eye care practitioners do not see every day because they are in people who do not access eye care.
Eye care practitioners see the burden of myopia in individuals every day: patients worrying about refractive changes; patients needing to update glasses and/or contact lenses to recover vision lost to myopia progression; patients with myopia-associated pathology and/or vision loss from those conditions; parents who worry about their children becoming myopic and progressing to higher levels of myopia, etc. These personal burdens also have some community-level implications via their effect on health expenditure, quality of life and productivity. However, the significant public health implications of myopia and high myopia are ones that clinical eye care practitioners do not see every day because they are in people who do not access eye care.
Vision impairment is associated with profound changes in quality of life and productivity.1-6 There are two main ways myopia can cause vision impairment, each of which can happen between regular visits to an eye care practitioner but are more common in people who never, or irregularly, attend for eye care. The first way myopia can cause vision impairment is via un- or under-corrected refractive error – distance vision impairment can result when a person with myopia is unable to obtain appropriate spectacles or contact lenses or have them updated as needed.7-10 Secondly, increasing myopia is associated with increasing prevalence of vision impairment from pathological complications including glaucoma and vitreoretinal diseases.11-13
It is broadly agreed that myopia is common and rapidly increasing over time.14,15 Interestingly, the demographics of people with myopia appears to be changing in two ways that are important in the link between myopia and vision impairment:10,13,14
- The “myopia epidemic” is “spreading” from countries with established, intense education systems, highly urbanized populations, and well-developed healthcare systems, to countries with fewer resources, and health systems that are less ready to deal with myopia and its complications;
- Myopia commonly starts in childhood and stays for life, so myopia is initially mostly in younger people when a country’s “myopia epidemic” begins, but then “spreads” to all age groups over decades.
There are barriers that prevent some people in any community from accessing adequate vision care and correction. Globally though, people are less likely to have sufficient optical correction, or access to healthcare able to adequately manage myopia complications, if they are older and/or live in rural areas of less developed countries.10,13 We have estimated that there were 480 million people worldwide in 2015 who experienced vision impairment from uncorrected myopia,10 and that there were 10 million people worldwide in 2015 who suffered vision impairment due to myopic macular degeneration.13 These estimates are substantially larger than vision impairment estimates for any other condition,9 suggesting that myopia was the leading cause of vision impairment in the world in 2015.
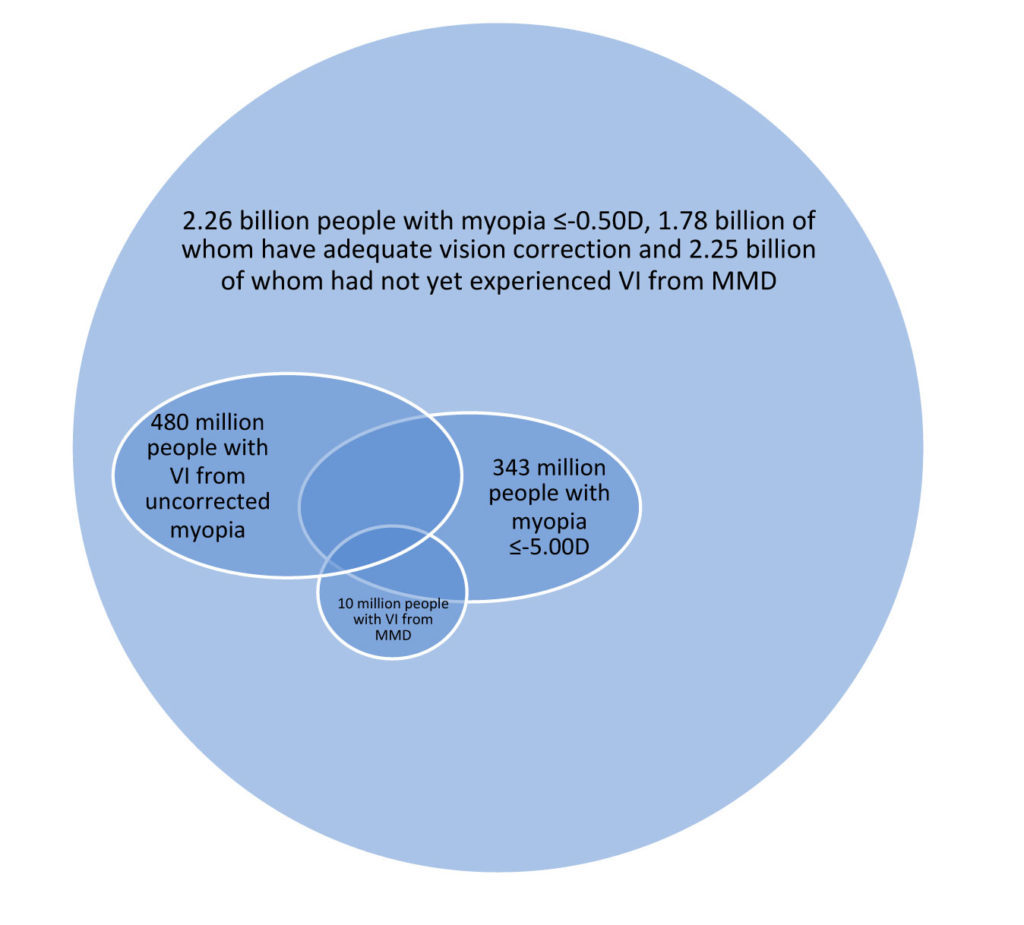
Figure 1. Number of people experiencing various myopia states in 2015 globally. VI = vision impairment. MMD = myopic macular degeneration.
But now it is 2019. Are these figures still relevant and what is likely to happen in the foreseeable future? Global prevalence of myopia and high myopia are almost certainly still increasing due to lifestyle factors.14 It is also probable that correction rates are rising as health systems and communities develop, and specific refractive care programs take effect.10 The rate of successful prevention of vision impairment from the pathological complications of myopia is probably also improving over time.13 The longitudinal global vision impairment data suggest that the balance of these factors probably means both the prevalence and number of people with vision impairment associated with myopia and high myopia is continuing and will continue, to rise over time unless we can change the paradigm.8,9
Implications: what do we need to do to limit and reverse the public health burden of myopia and high myopia? First, there is an urgent and massive need to improve access to refractive care, in each of our own communities, but particularly in low resource communities around the world. Second, there is an urgent and widespread need to do whatever we can to prevent and slow the progression of myopia – “visual hygiene” advice at the individual and community level, together with considered, evidence-based myopia management throughout life for all patients with myopia. That is, the public health burden of myopia and high myopia presents both immense challenges and great opportunities to the eye care community.

Tim Fricke, BOptom, MSc, senior research fellow with the Brien Holden Vision Institute
References
- Varma R, Wu J, Chong K, Azen SP, Hays RD, Los Angeles Latino Eye Study G. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology 2006; 113(10): 1846-53.
- Finger RP, Fenwick E, Marella M, et al. The impact of vision impairment on vision-specific quality of life in Germany. Investigative ophthalmology & visual science 2011; 52(6): 3613-9.
- Fenwick EK, Ong PG, Man RE, et al. Association of Vision Impairment and Major Eye Diseases With Mobility and Independence in a Chinese Population. JAMA ophthalmology 2016; 134(10): 1087-93.
- Foreman J, Dirani M, Taylor H. Refractive error, through the lens of the patient. Clin Exp Ophthalmol 2017; 45(7): 673-4.
- Fenwick EK, Ong PG, Man REK, et al. Vision impairment and major eye diseases reduce vision-specific emotional well-being in a Chinese population. The British journal of ophthalmology 2017; 101(5): 686-90.
- Mathers C, Ho J. Global Health Estimates Technical Paper – WHO methods and data sources for global burden of disease estimates 2000-2015. Geneva, Switzerland: Department of Information Evidence and Research, World Health Organization; 2017.
- Resnikoff S, Pascolini D, Mariotti S, Pokharel P. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bulletin of the World Health Organization 2008; 86(1): 63-70.
- Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 2017; 5(9): e888-e97.
- Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health 2017; 5(12): e1221-e34.
- Naidoo KS, Fricke TR, Frick KD, et al. Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis and modelling. Ophthalmology 2019; 126: 338-46.
- Tideman JW, Snabel MC, Tedja MS, et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA ophthalmology 2016; 134(12): 1355-63.
- Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet 2012; 379(9827): 1739-48.
- Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Brit J Ophthalmol 2018; 102(7): 855-62.
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016; 123(5): 1036-42.
- Modjtahedi BS, Ferris FL, 3rd, Hunter DG, Fong DS. Public Health Burden and Potential Interventions for Myopia. Ophthalmology 2018; 125(5): 628-30.













